2021 Outcomes Report (Dr. Warner):
One of the Core Values of our service is measurement and transparency. Thus, every year we review all surgical cases and report these publicly. Of course, conclusions as to durability of outcome cannot be made from this report; however, the depth and breadth of surgical cases is illustrated. Moreover, complication rates are reported, but ultimate outcome is not possible with such short follow-up. 2021 was unique in terms of the impact of COVID-19 on clinical volume.
Dr. Warner’s outcomes data is systematically reviewed by his Research Assistants utilizing the medical records system of Massachusetts General Hospital as well as our prospective Patient Reported Outcomes Database (SOS™, Arthrex, Naples, FL). Our methodology consisted of a review of all operations performed during the calendar year on a case-by-case basis, with special consideration made to procedure type, patient past surgical history (primary vs. revision status), and any complications arising during or after an operation. This data was collected, aggregated, and independently analyzed by the two Research Assistants with no direct input from the attending physician.
Physician Overview for the Year 2021
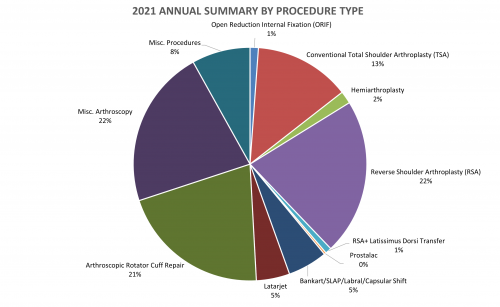
- 346 surgeries were performed throughout the year 2021
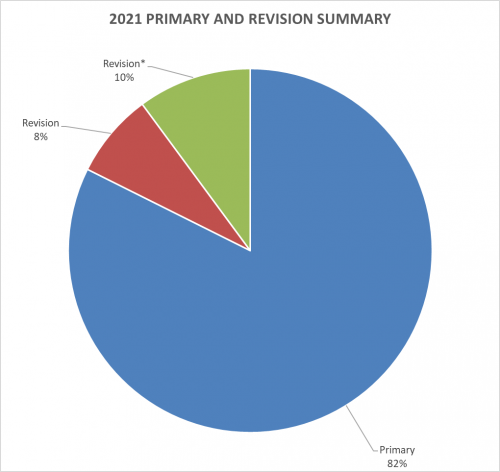
- Of these 346 operations, 285 were primary surgeries. Additionally, 26 were revisions of his own past cases (these revisions were performed in the 2021 calendar year, but the primary operation could be from prior years), and 35* were revisions of other surgeons’ cases.
2021 Surgeries Organized by type:
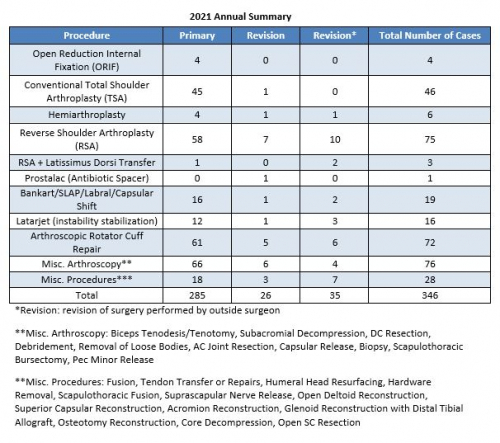
*Revision (green portion of above graph): revision of surgery performed by outside surgeon
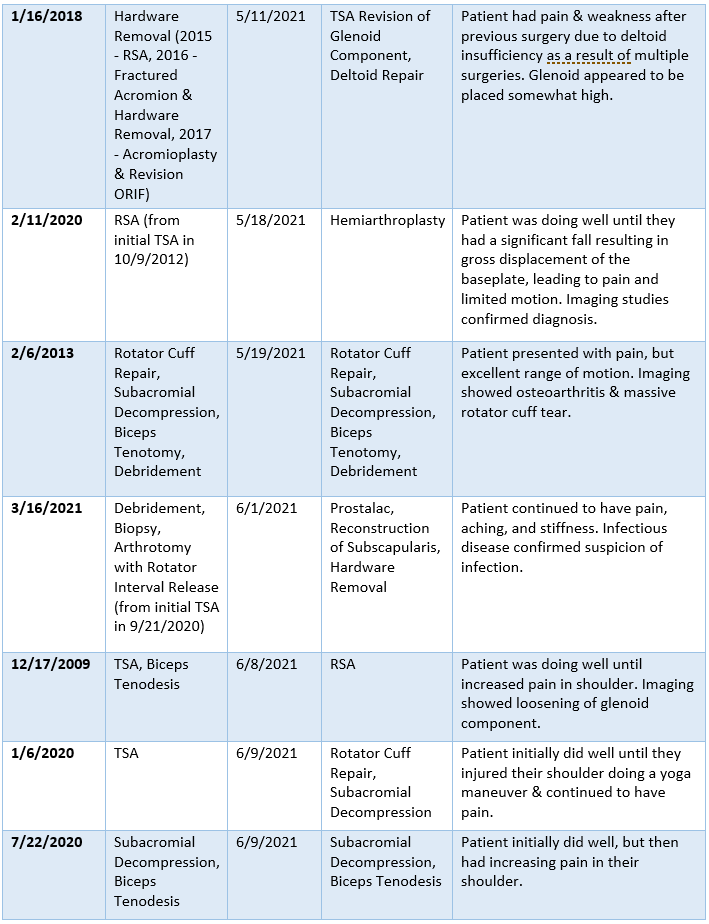
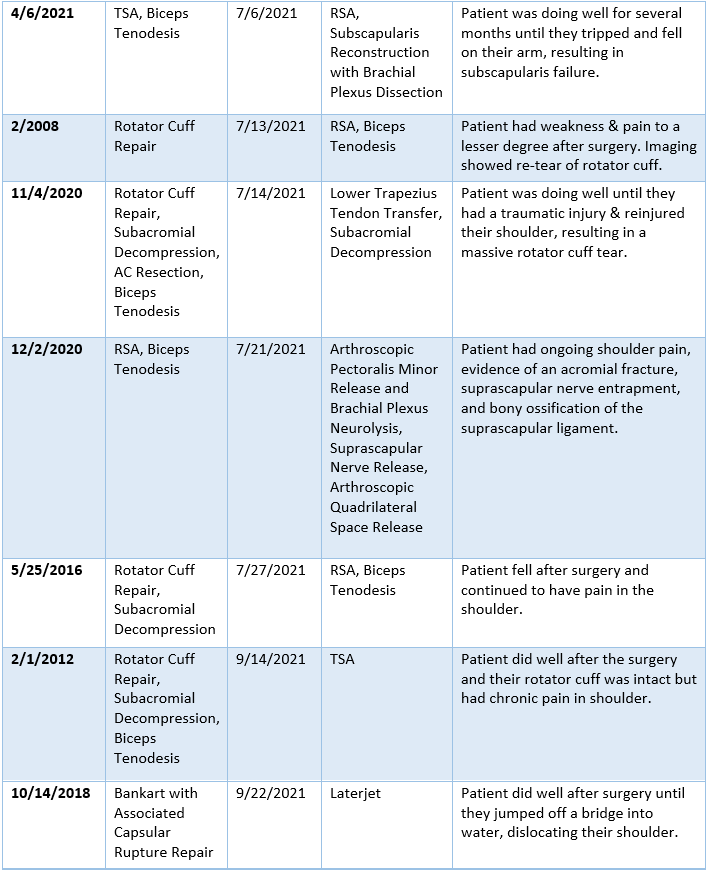
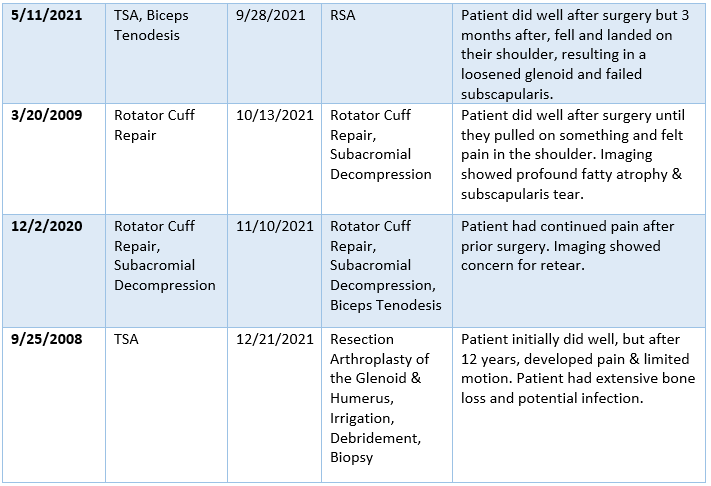
2021 Revision Timeline
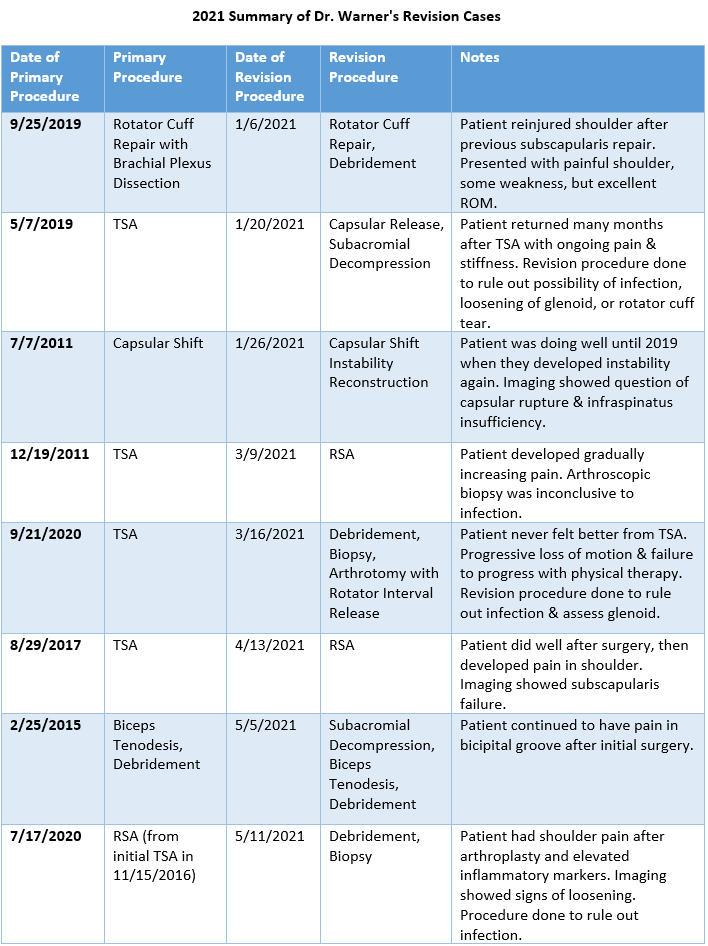
For the 8% of Dr. Warner’s cases that required a revision, the average length between the primary (index) and revision procedure was 4.6 years, ranging from 2.5 months to 13.4 years (red portion of the graph above). These revision procedures are summarized below:
2021 Summary of Dr. Warner’s Revision Cases
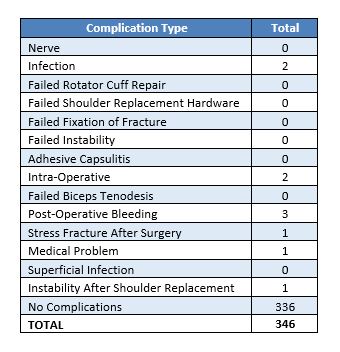
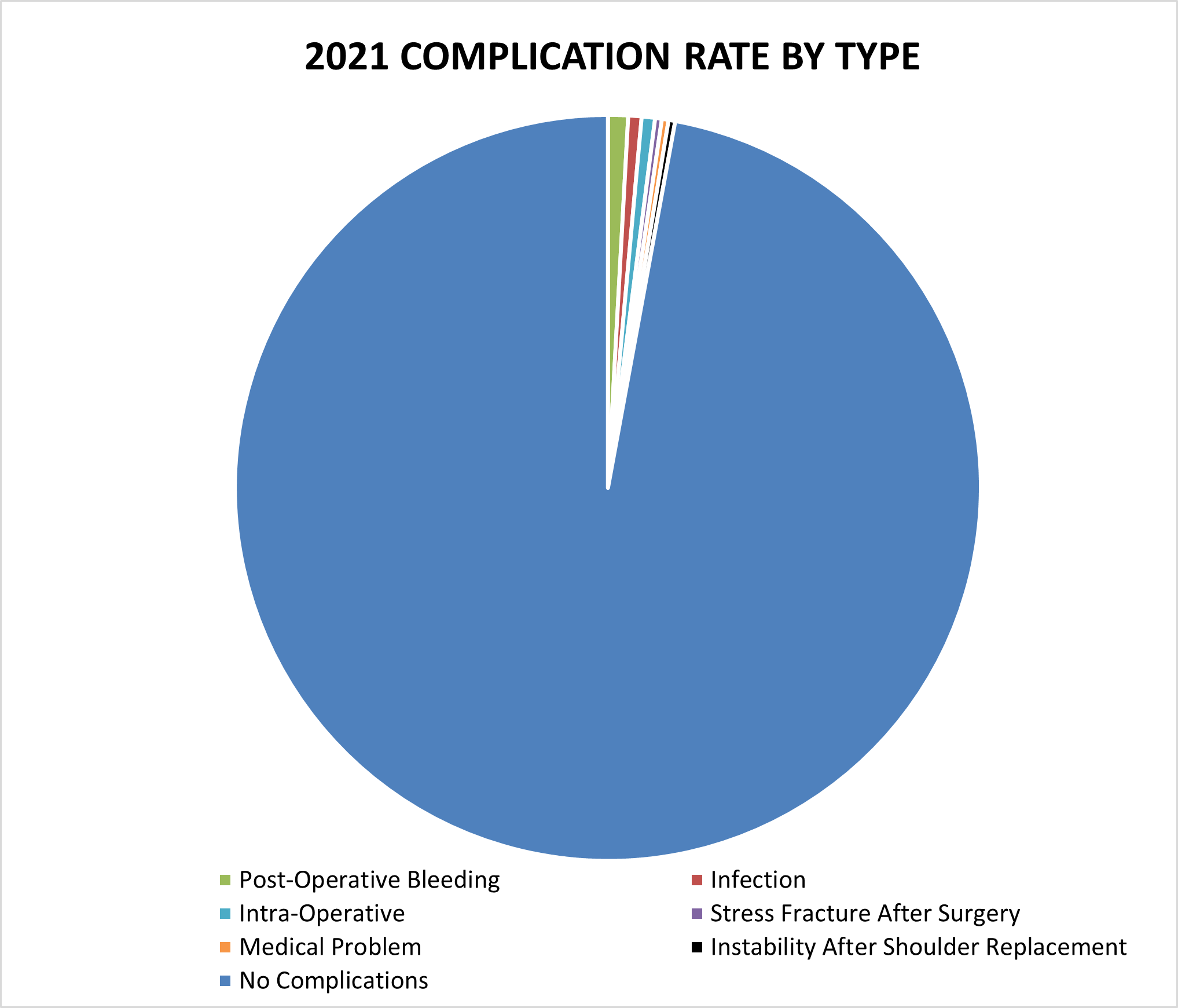
2021 Surgical Complications
Reported below are all of Dr. Warner’s complications during the 2021 calendar year. Of the 346 surgeries performed by Dr. Warner, 10 patients (2.9%) experienced a complication. These complications were identified in the calendar year 2021, but the primary operation could have occurred in prior years. Please see the data depicted below. Of note, post-operative bleeding constitutes the most prominent complication.
Management of Complications
Of all 346 surgeries in 2020, 7 cases (2.0%) had to be readmitted to the hospital for an additional operation. In the spirit of transparency and accountability, the Boston Shoulder Institute is providing details for each complication. This will enable patients to be fully informed as to risks of surgery. Each of Dr. Warner’s 2021 complications is detailed below, along with whether it is resolved or ongoing.
Of the 10 total cases, 6 have fully recovered and 4 have an ongoing problem. These are shown below in Green (recovered) and Red (not fully recovered).
A detailed recount of the readmissions follows:
- Post-Operative Bleeding
- Four days following a reverse shoulder arthroplasty, the patient began experiencing generalized weakness and lethargy. Patient was noted to be significantly anemic and was admitted to another hospital where they received a blood transfusion. Following transfusion, patient felt better and the hematoma was clearly resorbing. The patient reported their shoulder is relatively pain free.
- Following a reverse shoulder arthroplasty with latissimus dorsi tendon transfer, the patient began to experience swelling over the shoulder, mid-arm, and hand and a large hematoma with drainage from the incision. Three days after surgery, the patient underwent irrigation and debridement for post-operative hematoma. Following this surgery, the patient is doing well and is being treated with physical therapy.
- Two months following a revision of a hemiarthroplasty to a reverse shoulder arthroplasty, the patient’s incision appeared red and swollen. A month later, the patient noticed a blister over the incision that worsened with physical therapy. Extensive irrigation and debridement was performed to address the superficial draining wound. This is an ongoing issue, and the extent of final recovery is not yet known.
- Infection
- Two months following a total shoulder arthroplasty, the patient’s incision appeared red and swollen. Patient experienced pain and limited range of motion. Swelling persisted for another month with inflammatory markers suggesting infection. Six months after surgery, the patient underwent debridement and a biopsy showed evidence of infection. Patient received intravenous antibiotic therapy. Three months later, the shoulder replacement was removed and a Prostalac antibiotic spacer surgically inserted. Patient continued to take oral antibiotics. The infection seemed to be getting better, but the patient continued to have shoulder pain. This patient will soon undergo revision surgery to place a reverse shoulder replacement. Prognosis is good, but final recovery is not yet known.
- A little over one year following a reverse shoulder arthroplasty, the patient developed shoulder pain over the acromioclavicular (AC) joint. An initial AC joint injection was not helpful, but a second one provided relief. About 1.5 years after the initial operation, the patient developed a small red bump in front of the incision and underwent irrigation and debridement with biopsy, which demonstrated an infection. Patient took oral antibiotics but continued to have persistent infection and wound drainage. Change to a different oral antibiotics drainage resulted in elimination of drainage, and the patient is doing well.
- Instability After Shoulder Replacement
- Two weeks after a complex reverse shoulder arthroplasty, the patient woke up from sleep without sling, experiencing pain. X-ray showed dislocation of shoulder. They underwent a closed reduction under sedation. Following reduction, patient was immobilized in a sling and will start physical therapy. Patient will continue following-up as physical therapy progresses, and the final outcome is not yet determined.
- Medical Problem
- One month following a reverse shoulder arthroplasty, the patient was admitted to the hospital for swelling, redness, and pain from the shoulder to elbow. They were diagnosed with superficial thrombophlebitis in the cephalic vein and treated with Eliquis daily. This patient is recovering, and full recovery is expected.
Itemized details for the remaining complications that did not require readmission are as follows:
- Intra-Operative
- Capsular Release: During surgery, the hook tip of a radiofrequency device used during the operation broke. An x-ray showed the 2 mm small metal piece remained lodged extra-articularly in the soft tissues. The metal was left in the position because it would not cause any harm while removal would cause more harm. The operation was successful in restoring range of motion and the patient is being treated with physical therapy, recovering well. This patient is happy with the outcome and has improved range of motion and strength.
- Reverse Shoulder Arthroplasty: As a result of rotator cuff stiffness, an intra-operative greater tuberosity fracture occurred from the lateralization of the reduction. The tuberosity was repaired. The patient developed post-surgical stiffness, and x-rays demonstrated displacement of a small fragment of the tuberosity blocking motion. The patient is considering surgery to remove the bony fragment to improve their motion. While the patient has minimal pain, they are considering surgery to remove the bony fragment to improve their motion.
- Stress Fracture After Surgery
- Reverse Shoulder Arthroplasty: Three months after surgery, the patient was getting into a car and felt a snap followed by pain and swelling, resulting in an acromion stress fracture. The patient’s shoulder was immobilized in a sling for 10 weeks, after which they noted minimal pain. This patient is now very happy with the outcome.
