2022 Outcomes Report (Dr. Warner)
One of the Core Values of our service is measurement and transparency. Thus, every year we review all surgical cases and report these publicly. Of course, conclusions as to durability of outcome cannot be made from this report; however, the depth and breadth of surgical cases is illustrated. Moreover, complication rates are reported, but ultimate outcome is not possible with such short follow-up.
Dr. Warner’s outcomes data is systematically reviewed by his Research Assistants utilizing the medical records system of Massachusetts General Hospital as well as our prospective Patient Reported Outcomes Database (SOS™, Arthrex, Naples, FL). Our methodology consisted of a review of all operations performed during the calendar year on a case-by-case basis, with special consideration made to procedure type, patient past surgical history (primary vs. revision status), and any complications arising during or after an operation. This data was collected, aggregated, and independently analyzed by the two Research Assistants with no direct input from the attending physician.
Physician Overview for the Year 2022
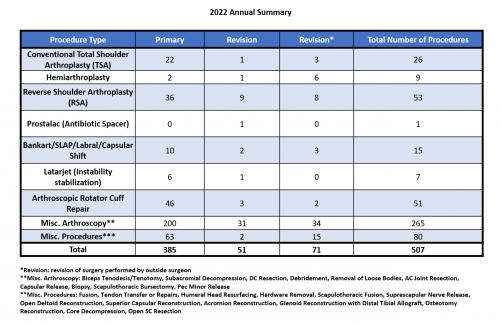
1. 507 procedures were performed throughout the 2022 calendar year.
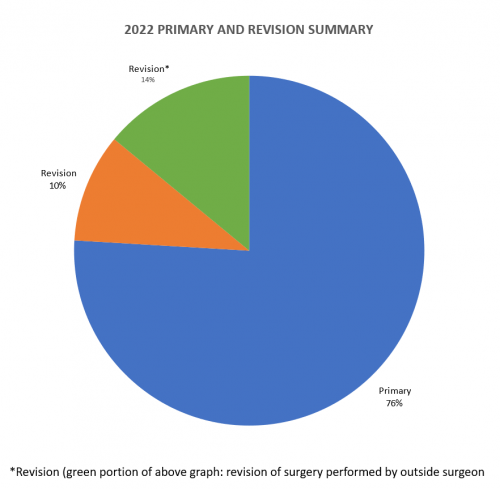
2. Of these 507 procedures, 385 were primary surgeries. Additionally, 51 were revisions of his own past cases (these revisions were performed in the 2022 calendar year, but the primary operation could be from prior years), and 71* were revisions of other surgeons’ cases.
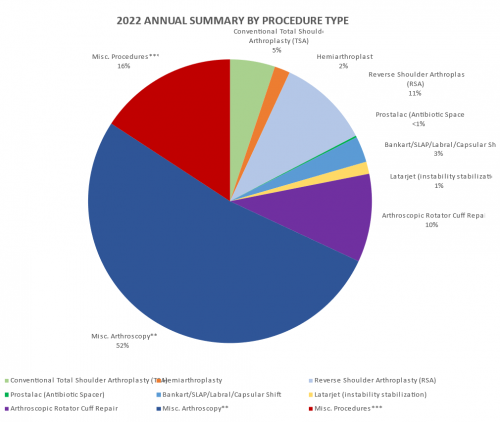
2022 Surgeries Organized by Type:
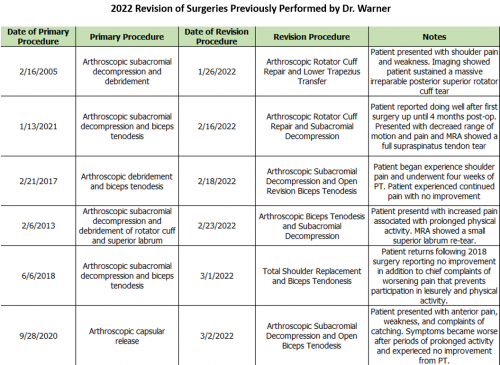
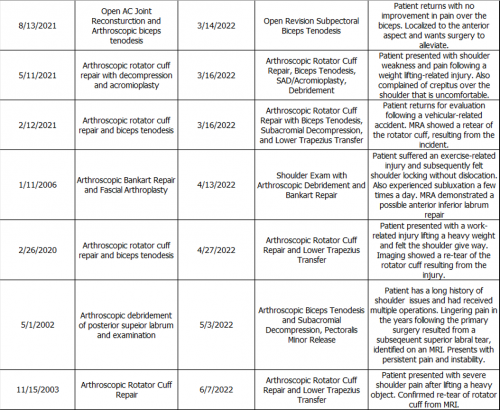
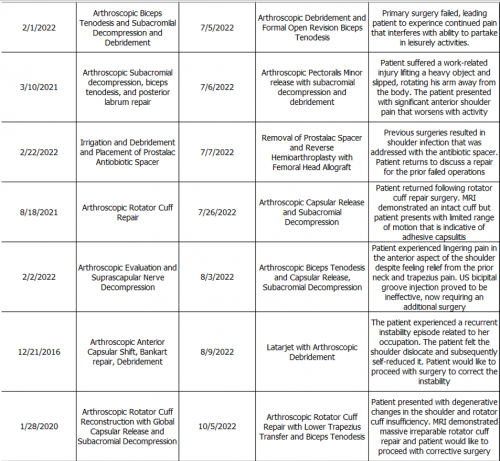
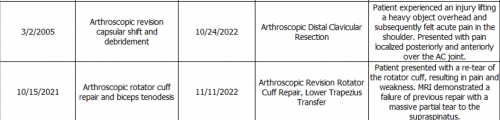
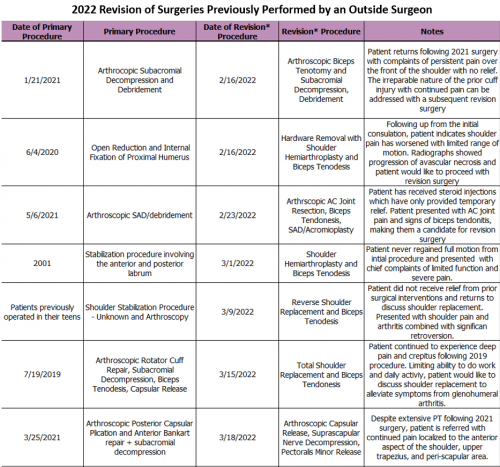
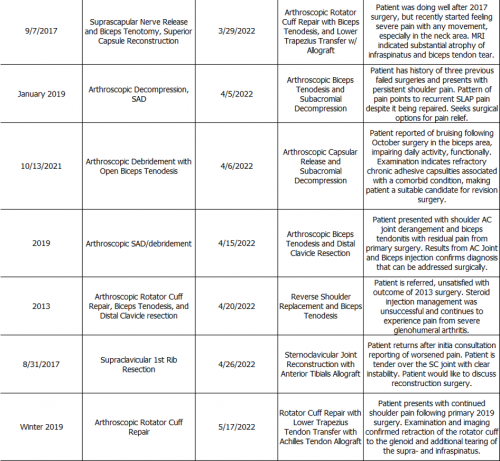
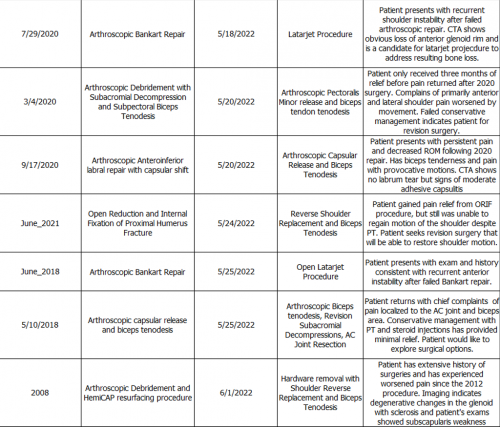
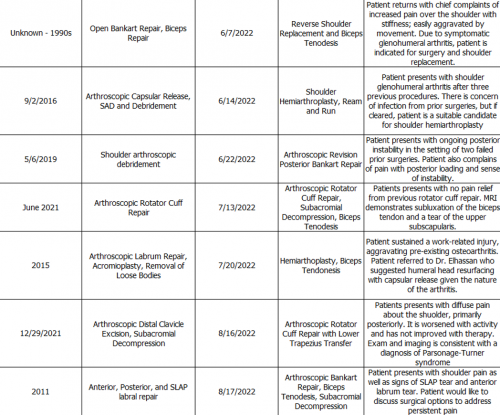
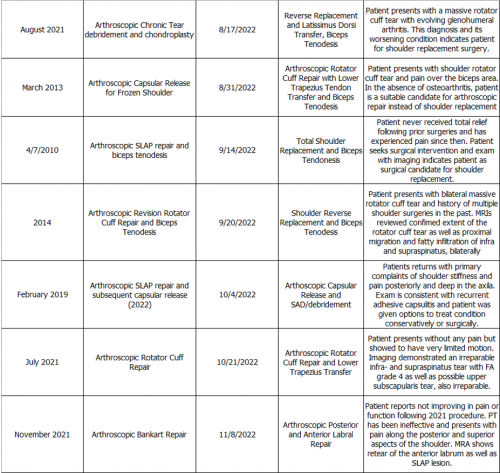
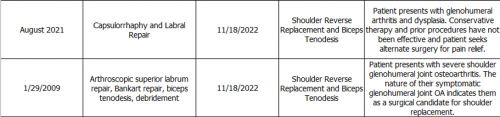
2022 Revision Timeline
For the 24% of Dr. Warner’s total procedures that were classified as a revision, the average length between the primary (index) and revision procedure was 5.5 years, ranging from 4.2 months to 25 years (green and orange portion of the graph above). These revision procedures are summarized below:
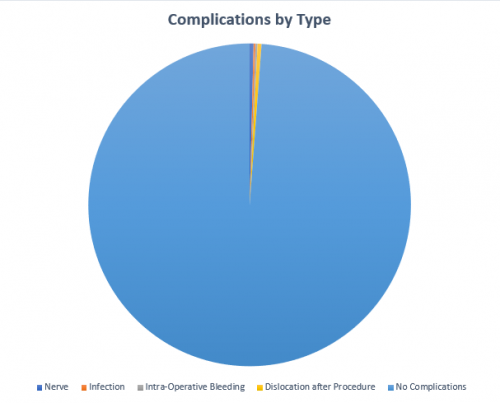
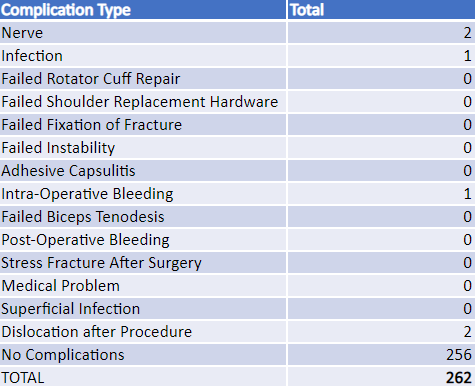
2022 Surgical Complications
Reported below are all of Dr. Warner’s complications during the 2022 calendar year. Of the 262 patients operated on by Dr. Warner, 6 patients (2.3%) experienced a complication. These complications were identified in the calendar year 2022, but the primary operation could have occurred in prior years. Please see the complication summary depicted below.
Management of Complications
Of all the 262 patients in 2022, 3 (1.15%) had to be readmitted to the hospital for an additional operation. In the spirit of transparency and accountability, the Boston Shoulder Institute is providing details for each complication. This will enable patients to be fully informed as to the risks of surgery. Each of Dr. Warner’s 2022 complications is detailed below, along with whether it is resolved or ongoing.
Of the 6 total cases, 1 has fully recovered and 5 have an ongoing problem. These are shown below in Green (recovered) and Red (not fully recovered).
A detailed recount of readmissions follows:
Nerve
This patient has diabetes and was stiff after a Latarjet procedure. He underwent an arthroscopic release of adhesions due to refractory adhesive capsulitis. He is currently undergoing PT and improving.
Dislocation after procedure
This patient experienced a dislocation of the shoulder 6 months after a Latarjet procedure. This patient will be undergoing a revision surgery to remove the broken bone graft and replace it with a distal tibial allograft.
Infection
This patient experienced an infection after a reverse shoulder replacement. He underwent a surgical debridement and is recovering now with good pain relief and improving function.
Itemized details for the remaining complications that did not require readmission are as follows:
Nerve
This patient had weakness and numbness after a Latarjet procedure. At 6 months this nerve problem resolved but patient was continuing to complain of pain. She is considering revision surgery due to mechanical symptoms and pain. This would involve neurolysis (release of scar around nerve and revision of Latarjet to bone graft for the glenoid socket.
Dislocation after procedure
Patient has ongoing pain after reverse shoulder replacement. Patient is waiting to see if additional surgery is necessary.
Intraoperative Bleed
Patient experienced bleeding during shoulder replacement surgery. Patient then underwent repair of the blood vessel and has improved to the point where he wants to reschedule his shoulder replacement.
