2019 Outcomes Report (Dr. Warner):
Dr. Warner’s outcomes data was systematically reviewed by his two Research Assistants utilizing the medical records system of Massachusetts General Hospital. Our methodology consisted of a review of all operations performed during the calendar year on a case-by-case basis, with special consideration made to procedure type, patient past surgical history (primary vs. revision status), and any complications arising during an operation. This data was collected, aggregated, and analyzed by the two Research Assistants with no direct input from the attending physician.
Physician Overview for the Year 2019
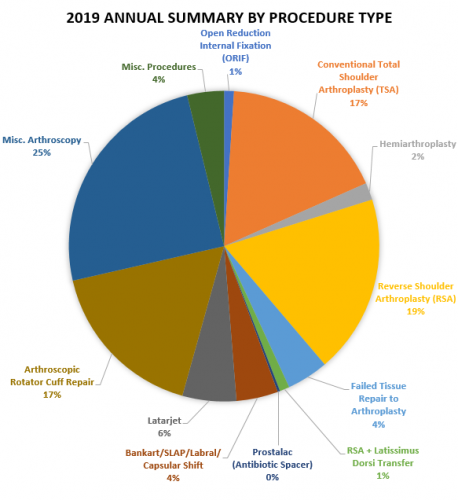
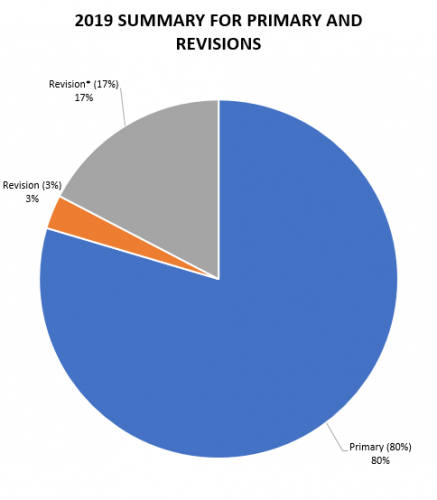
- 392 surgeries were performed throughout the year 2019
- Of these 392 operations, 12 were revisions of his own past cases (these revisions were performed in the 2019 calendar year, but the primary operation could be from prior years), and 68* performed were revisions of other surgeons’ cases. Additionally, 312 were primary surgeries.
2019 Surgeries Organized by type:
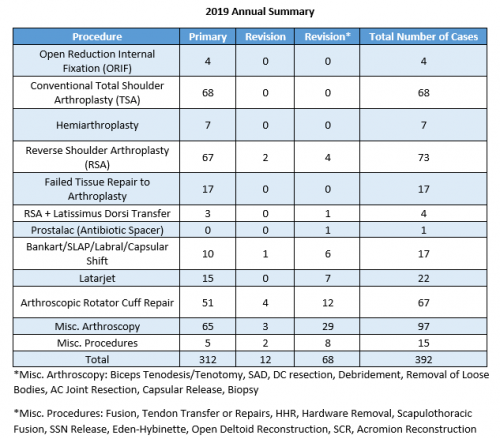
*Revision of surgery performed by outside surgeon
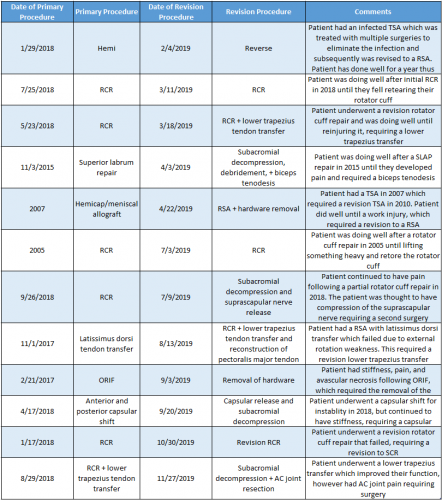
2019 Summary Revision Timeline
For the 3% of Dr. Warner’s cases that required a revision, the average length between the primary and revision procedure was 37.5 months (3.2 years), ranging from 8 months to 168 months (0.66 years- 14 years). These revision procedures are summarized below:
2019 Surgical Complications
Reported below are all of Dr. Warner’s complications during the 2019 calendar year. Of the 392 surgeries performed by Dr. Warner, 14 patients (3.5%) experienced a complication. These complications were identified in the calendar year 2019, but the primary operation could have occurred in prior years. Please see the data depicted below. Of note, nerve injuries constitute the most prominent complication.
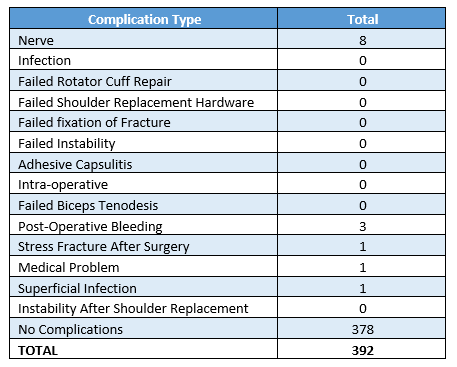
*Note: One of the complications listed under “Nerve” had additional complications including a DVT (blood clot) and hematoma (post-operative bleeding), resulting in hospital readmission.
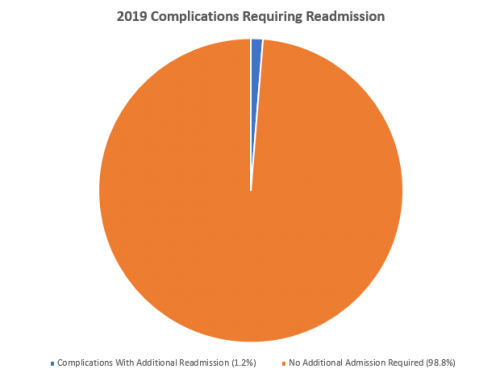
Management of Complications
Of all 392 surgeries in 2019, 5 cases (1.2%) had to be readmitted to the hospital for management. Only one of those patients required an additional operation (0.25%). In the spirit of transparency and accountability, the Boston Shoulder Institute is providing details for each complication. This will enable patients to be fully informed as to risks of surgery. Each of Dr. Warner’s 2019 complications is detailed below, along with whether it is resolved or ongoing. Of the 5 readmissions, all complications have fully resolved without residual problems for the patients.
A detailed recount of readmissions follows:
A patient was readmitted for a right subclavian and axillary DVT (blood clot) and hematoma (post-operative bleeding) that required drainage following a Latarjet procedure. The patient was also diagnosed with axillary nerve dysfunction. All complications have been resolved and the patient has fully improved.
After a reverse shoulder arthroplasty, the patient developed a hematoma (post-operative bleeding). The patient retuned to the hospital and an incisional wound vac was placed for three days. The problem has since resolved.
After a sternoclavicular joint reconstruction, the patient presented back to the hospital with shortness of breath and was diagnosed with pulmonary embolisms in both lungs. The patient was placed on therapeutic anticoagulation and the problem has since resolved.
The patient returned to the hospital three weeks following a reverse shoulder arthroplasty and was found to have a large hematoma (post-operative bleeding). An incisional wound vac was placed for 72 hours, and the problem has since resolved.
Following a rotator cuff repair, a patient was readmitted to the hospital due to nausea, vomiting, and low sodium levels. The patient spent three days in the ICU and was treated by their PCP with intravenous fluids. All the above has been resolved.
Itemized details for the remaining complications that did not require readmission are as follows:
Nerve
Summary: All of the complications were temporary stretch injuries. Six out of seven complications listed below have fully resolved and the patients are doing well.
Total Shoulder Arthroplasty: Patient was experiencing decreased sensation in the axillary nerve and weakness in their deltoid. An EMG confirmed axillary nerve neuropraxia (stretch injury) and was treated with physical therapy. RESOLVED
Latarjet: Patient was experiencing weakness in the deltoid as a result of axillary neuropraxia (stretch injury). This was treated with physical therapy. RESOLVED
Reverse Shoulder Arthroplasty: Patient complained of numbness and tingling in the small and ring finger after their surgery as a result of ulnar nerve neuropraxia (stretch injury). This was treated with physical therapy. RESOLVED
Reverse Shoulder Arthroplasty: Patient was experiencing weakness in their deltoid and an EMG revealed axillary nerve neuropraxia (stretch injury). This was treated with physical therapy. RESOLVED
Reverse Shoulder Arthroplasty: Patient was experiencing numbness and weakness in their first three digits shortly following surgery. An EMG was obtained and revealed axillary nerve dysfunction and anterior interosseous nerve palsy (nerve to the forearm). This was treated with physical therapy. RESOLVED
Latarjet: Following surgery, the patient began experiencing an axillary and musculocutaneous nerve injury. This was treated with physical therapy. RESOLVED
Reverse Shoulder Arthroplasty: Following surgery, the patient began experiencing wrist drop (inability to hold wrist up) and the inability to extend their fingers, caused by radial nerve neuropraxia (stretch injury). The patient is improving with occupational therapy. ONGOING
Superficial Infection
Reverse Shoulder Arthroplasty: After surgery, patient had some drainage from the incision and there was a concern for infection. However, this completely cleared up and the wound is benign with no erythema, no warmth, and no tenderness. RESOLVED
Stress Fracture
Reverse Shoulder Arthroplasty: Three months following surgery, the patient began experiencing shoulder pain and was found to have an acromion fracture. The fracture was treated conservatively with a sling and has since healed and resolved. RESOLVED
