- Reverse Total Shoulder Replacement Module
- Patient Testimonials: Reverse Total Shoulder Replacement
- Reverse Total Shoulder Replacement: Post-Operative Information
- Reverse Total Shoulder Replacement with Latissimus Transfer: Post-Operative Information
Outcomes following Reverse Prosthesis:
Eric Black, MD; Paul Yannopoulos, BA; Jon Warner, MD
There are many studies in the literature that show good to excellent outcomes for patients who have a reverse total shoulder arthroplasty. These can be seen found at the bottom of this page, and at the bottom of the page regarding patient information for reverse Overall, most patients can expect to have significant improvements in range of motion (especially if stiff before surgery) as well as improvements in pain. Typically, most studies quote patient satisfaction rates >90%. In general, outcomes are higher for patients undergoing a primary surgery when compared to a revision surgery.
Outcomes – Our Experience
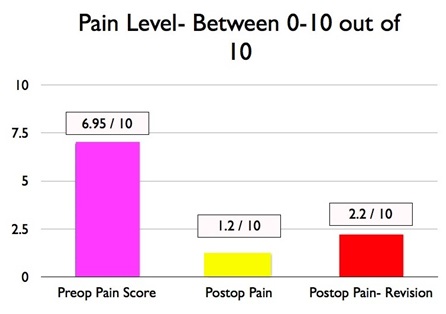
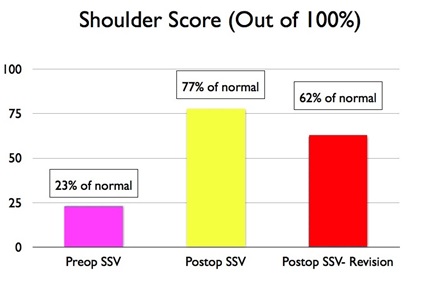
In reviewing the Boston Shoulder Institute experience from 2004-2011, we found that patients pain and shoulder function scores improved significantly in patients who had a reverse shoulder arthroplasty. We reviewed 230 patients and this data was determined 2 years after surgery to ensure that findings were constant. On average, patients complained of pain at 6.9 out of 10 on the 10-point pain scale prior to surgery. After surgery, patients’ average pain was 1.2 out of 10 in primary cases, and 2.1 out of 10 in revision cases.
Prior to surgery, patients rated their shoulder function scores on average at 26% of normal (out of 100%). Greater than two years after surgery, patients rated their shoulder function at an average of 77% after a primary surgery, and 61% after a revision surgery. This is an average of a 50% improvement in function and 5 points less on the pain scale!!!
 Complications and Risks:
Complications and Risks:
Unfortunately there are risks and complications that are both common to all joint replacements and unique to the reverse prosthesis.
- Bleeding is typically managed with blood transfusions, and there is a roughly 15-25% chance that patients will require a blood transfusion. (Millet PJ, Porramatikul M, Chen N, Zurakowski D, Warner JJ. Analysis of transfusion predictors in shoulder arthroplasty. J Bone Joint Surg Am. 2006. 88(6):1223-30.http://www.ncbi.nlm.nih.gov/pubmed/16757754)
- Infection is also a possibility, and patients will receive antibiotics for 24 hours following surgery to prevent the risk of infection. We also take multiple measures during surgery to minimize risk, including occlusive draping with iodine impregnated drapes, special prep solution, more rapid surgery (with experience), and occlusive dressing. If a reverse prosthesis becomes infected, this is usually managed by staged revision surgeries. See our Prostalac Module for further information.
- Failure of the reverse components (loosening or pullout of screws) is unique to the reverse prosthesis, and can be managed by a revision of the components.
- Dislocation of a prosthesis can be treated oftentimes with a reduction of the dislocation under anesthesia. This is successful as a definitive treatment especially if the dislocation occurs shortly after the original surgery.
- Nerve injury is rare, and is usually treated with watchful waiting for return of function. If no function returns, patients may undergo explorations of the involved nerves and tendon transfers to improve function.
- Fractures – fractures of the surrounding bones may occur in patients with weak bones. Depending on the location of the fracture, patients may be treated with or without surgery.
Complications – Our Experience:
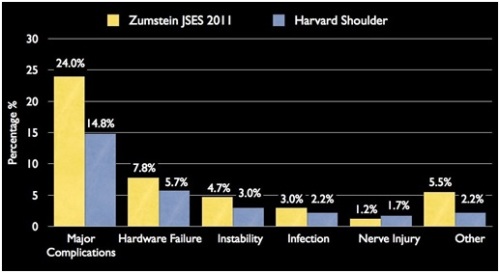
We recently reviewed all patients who underwent reverse shoulder replacements (including primary and revision surgeries). The overall major complication rate was 15%. This is similar to (if not less than) many other reports in the literature describing complication rates after reverse shoulder replacement. One recent report included a summary analysis of many different studies and found an average complication rate of 24% in the literature. (Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. Journal of Shoulder and Elbow Surgery 2011;20:146–157. http://www.ncbi.nlm.nih.gov/pubmed/21134666)
The rate of complications is lower for patients who have not had a prior shoulder replacement (10%), when compared to patients undergoing a revision surgery and having a reverse prosthesis (22%). Complications included (and are listed in order of most to least frequent)
- Failure of the prosthesis
- Rate: 5.7% of total (4.9% in primary surgery, 6.9% in revision surgery)
- Instability – dislocation of the prosthesis which typically did not require a revision of the prosthesis
- Rate: 3% of total (2.1% in primary surgery, 4.6% in revision surgery)
- Infection
- Rate: 2% of total (1.4% in primary surgery, 3.4% in revision surgery)
- Nerve injury
- Rate: 1.7% of total (0.7% in primary surgery, 3.4% in revision surgery)
- Other major complications (including bleeding, need for hardware removal due to irritation)
- Rate: 2.1% of total (1.4% in primary surgery, 3.4% in revision surgery)
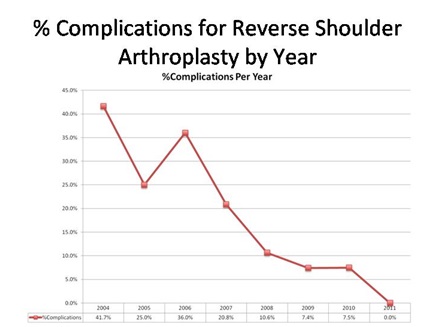
Below is a graph illustrating the decrease in complication rates per year by our senior surgeons, Dr. Warner and Dr. Higgins.
Boston Shoulder Institute Complication Rate Compared to Historical Literature:
LITERATURE:
- Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology.The Journal of Bone and Joint Surgery2007;89:1476–1485.
- Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br2004;86:388–395.
- Nolan BM, Ankerson E, Wiater JM.Reverse total shoulder arthroplasty improves function in cuff tear arthropathy.Clin Orthop Relat Res 2011;469:2476–2482.
- Roy J-S, Macdermid JC, Goel D, Faber KJ, Athwal GS, Drosdowech DS. What is a Successful Outcome Following Reverse Total Shoulder Arthroplasty?Open Orthop J2010;4:157–163.
- Cazeneuve J-F, Cristofari D-J.The reverse shoulder prosthesis in the treatment of fractures of the proximal humerus in the elderly.J Bone Joint Surg Br 2010;92:535–539.
- Austin L, Zmistowski B, Chang ES, Williams GR.Is reverse shoulder arthroplasty a reasonable alternative for revision arthroplasty?Clin Orthop Relat Res 2011;469:2531–2537.