2020 Outcomes Report (Dr. Warner):
One of the Core Values of our service is measurement and transparency. Thus, every year we review all surgical cases and report these publicly. Of course, conclusions as to durability of outcome cannot be made from this report; however, the depth and breadth of surgical cases is illustrated. Moreover, complication rates are reported, but ultimate outcome is not possible with such short follow-up. 2020 was unique in terms of the impact of COVID-19 on clinical volume.
Dr. Warner’s outcomes data is systematically reviewed by his Research Assistants utilizing the medical records system of Massachusetts General Hospital as well as our prospective Patient Reported Outcomes Database (SOS™, Arthrex, Naples, Fl). Our methodology consisted of a review of all operations performed during the calendar year on a case-by-case basis, with special consideration made to procedure type, patient past surgical history (primary vs. revision status), and any complications arising during or after an operation. This data was collected, aggregated, and independently analyzed by one Research Assistant with no direct input from the attending physician.
Physician Overview for the Year 2020
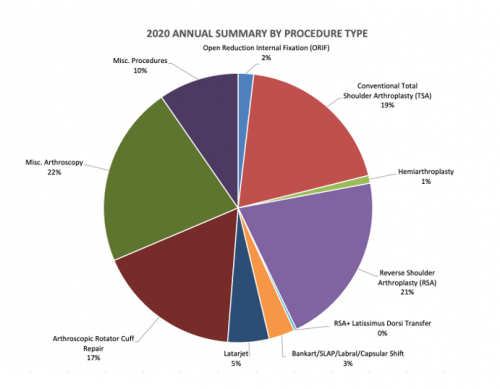
- 322 surgeries were performed throughout the year 2020
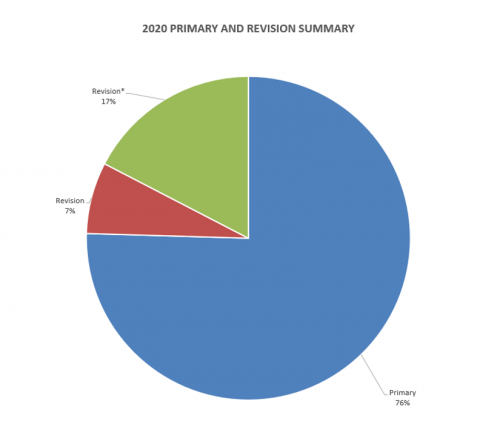
- Of these 322 operations, 243 were primary surgeries. Additionally, 23 were revisions of his own past cases (these revisions were performed in the 2020 calendar year, but the primary operation could be from prior years), and 56* were revisions of other surgeons’ cases.
2020 Surgeries Organized by type:
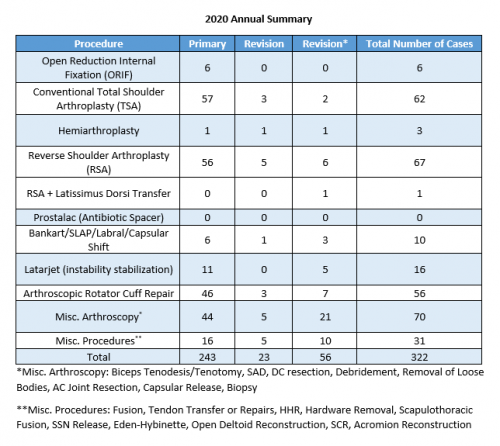
Revision*(Green Portion of Above Graph)= Revision of surgery performed by outside surgeon
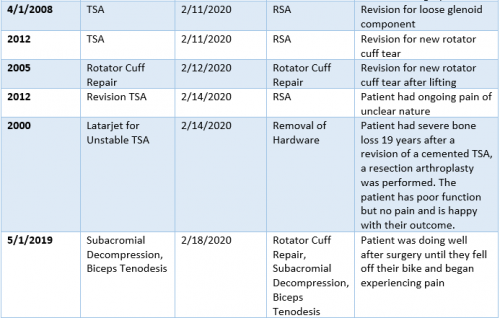
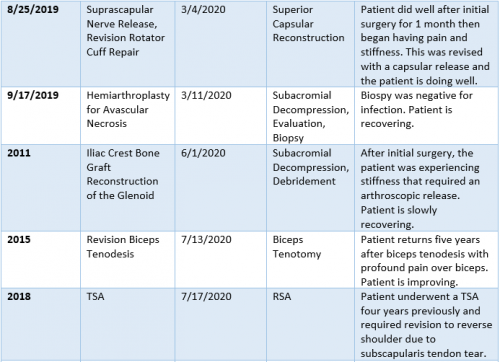
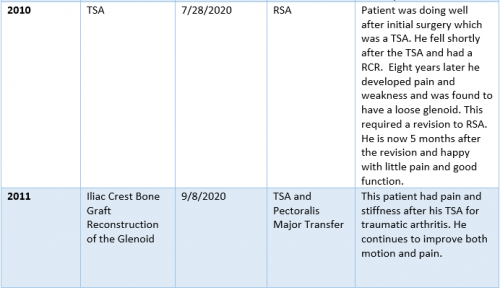
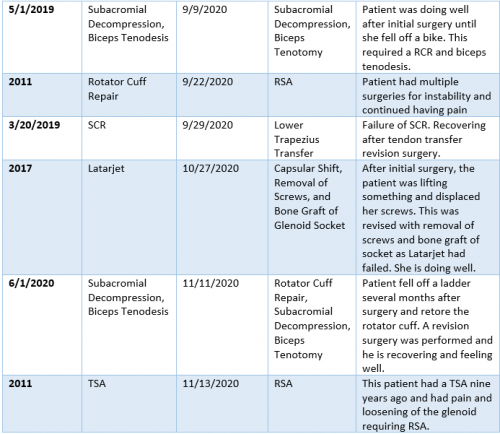
2020 Revision Timeline
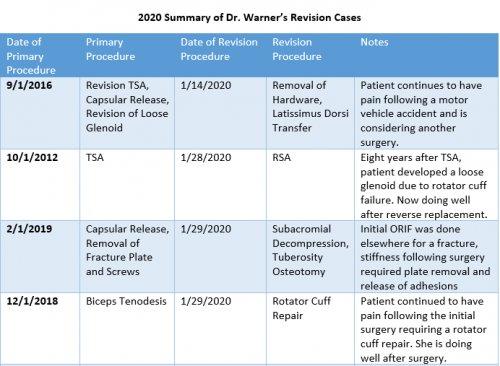
For the 7% of Dr. Warner’s cases that required a revision, the average length between the primary (index) and revision procedure was 6.1 years, ranging from 5 months to 20 years (red portion of the graph above). These revision procedures are summarized below:
2020 Summary of Dr. Warner’s Revision Cases
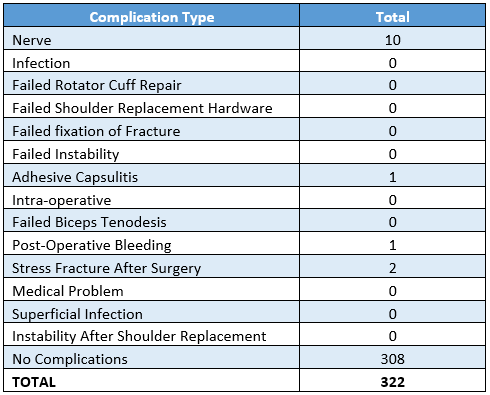
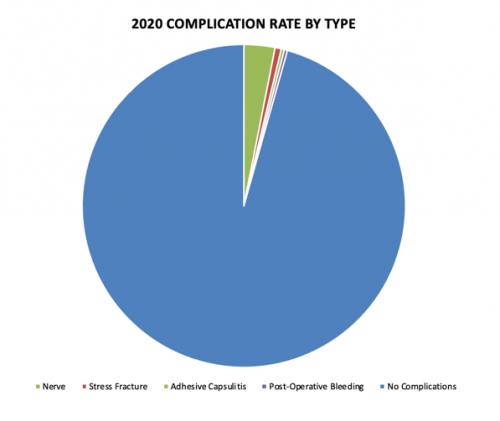
2020 Surgical Complications
Reported below are all of Dr. Warner’s complications during the 2020 calendar year. Of the 322 surgeries performed by Dr. Warner, 14 patients (4.2%) experienced a complication. These complications were identified in the calendar year 2020, but the primary operation could have occurred in prior years. Please see the data depicted below. Of note, nerve dysfunction constitutes the most prominent complication.
Management of Complications
Of all 322 surgeries in 2020, 1 case (0.3%) had to be readmitted to the hospital for an additional operation. In the spirit of transparency and accountability, the Boston Shoulder Institute is providing details for each complication. This will enable patients to be fully informed as to risks of surgery. Each of Dr. Warner’s 2020 complications is detailed below, along with whether it is resolved or ongoing.
A detailed recount of the readmission follows:
- Two weeks following a Latarjet procedure, the patient began experiencing increasing swelling, pain, and a large hematoma (post-operative bleeding). They required another operation to evacuate the hematoma. Following this surgery, the patient reported no pain or swelling, and the complication has completely resolved.
Itemized details for the remaining complications that did not require readmission are as follows:
- Nerve
- Reverse Shoulder Arthroplasty: Following surgery, the patient noticed poor motion and weakness. An EMG showed brachial plexus dysfunction and was treated conservatively with physical therapy. RESOLVED
- Reverse Shoulder Arthroplasty: After surgery, the patient began developing numbness, tingling, and decreased motion in their hand and wrist. An EMG demonstrated brachial plexus lower trunk palsy. The patient is being treated with occupational therapy. At 4 months after surgery the patient’s function is recovering. RECOVERING
- Reverse Shoulder Arthroplasty: The day after surgery, the patient felt numbness in their hand and was unable to extend their fingers and wrist. An EMG indicated brachial plexus stretch injury. The patient was fitted with a splint and will continue following-up. ONGOING
- Total Shoulder Arthroplasty: The patient was unable to move their wrist and fingers following surgery. An EMG confirmed radial nerve dysfunction. The patient was given a splint and treated with occupational therapy. Three months after their surgery they noted an improvement of symptoms and will continue following-up. RESOLVED
- Reverse Shoulder Arthroplasty: After surgery, the patient was unable to use their hand. They began using a wrist brace and was treated with occupational therapy. An EMG confirmed radial nerve neuropathy. Three months after surgery, the patient reports improved symptoms and will continue following-up. RECOVERING
- Total Shoulder Arthroplasty: The patient was unable to move their wrist and hand after surgery. They were fitted with a splint and treated conservatively. The patient completely recovered three months following surgery. RESOLVED
- Total Shoulder Arthroplasty: Patient developed uncomfortable sensation and reduced function of their hand following surgery. An EMG confirmed brachial plexopathy. The patient underwent an ulnar nerve release and is improving. RECOVERING
- Reverse Shoulder Arthroplasty: The patient began experiencing pain and numbness in their fingers following surgery. Motor function was normal. The patient was given a wrist splint and treated with physical therapy. Patient has only been seen virtually due to COVID-19. RECOVERING
- Total Shoulder Arthroplasty: Following surgery, the patient noted decreased axillary nerve sensation and weakness. They also suffered several falls in his home. An EMG confirmed axillary nerve neuropraxia (stretch injury). The patient is doing surgery and has evidence of a subscapularis tendon failure though deltoid function is recovering. RECOVERING
- Reverse Shoulder Arthroplasty: The patient could not move their wrist following surgery and began wearing a brace. An EMG demonstrated radial nerve palsy and cervical radiculopathy. At most recent evaluation 2 months after surgery hand function is improving. RECOVERING
- Adhesive Capsulitis:
- Latarjet: One month following surgery, the patient returned to the office with significant stiffness and loss of motion. They were treated with physical therapy with no improvement. A capsular release and a release of the quadrilateral space was performed and the patient is improving. RECOVERING
- Stress Fracture
- Reverse Shoulder Arthroplasty: Four months after surgery, the patient began having pain and a limited range of motion. It was found they had an acromion stress fracture and was treated with sling immobilization. RESOLVED
- Reverse Shoulder Arthroplasty: Five months after surgery, the patient began developing pain and a CT scan revealed an acromion stress fracture. They were treated with sling immobilization. RESOLVED
