2022 Outcomes Report (Dr. Elhassan)
One of the Core Values of our service is measurement and transparency. Thus, every year we review all surgical cases and report these publicly. Of course, conclusions as to durability of outcome cannot be made from this report; however, the depth and breadth of surgical cases is illustrated. Moreover, complication rates are reported, but ultimate outcome is not possible with such short follow-up.
Dr. Elhassan’s outcomes data is systematically reviewed by his Research Assistants utilizing the medical records system of Massachusetts General Hospital as well as our prospective Patient Reported Outcomes Database (SOS™, Arthrex, Naples, FL). Our methodology consisted of a review of all operations performed during the calendar year on a case-by-case basis, with special consideration made to procedure type, patient past surgical history (primary vs. revision status), and any complications arising during or after an operation. This data was collected, aggregated, and independently analyzed by the two Research Assistants with no direct input from the attending physician.
Physician Overview for the Year 2022
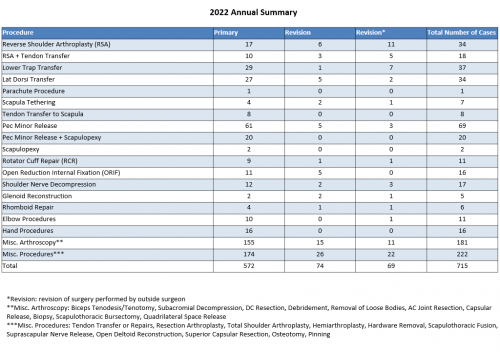
1. 715 procedures were performed throughout the 2022 calendar year.
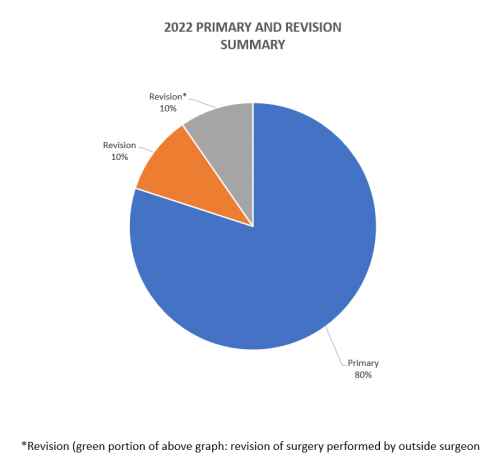
2. Of these 715 procedures, 572 were primary surgeries. Additionally, 74 were revisions of his own past cases (these revisions were performed in the 2022 calendar year, but the primary operation could be from prior years), and 69* were revisions of other surgeons’ cases.
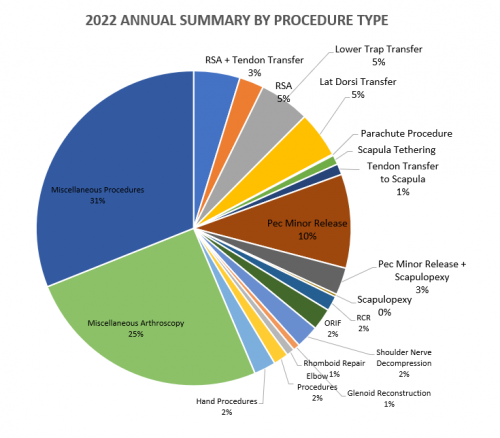
2022 Surgeries Organized by Type:
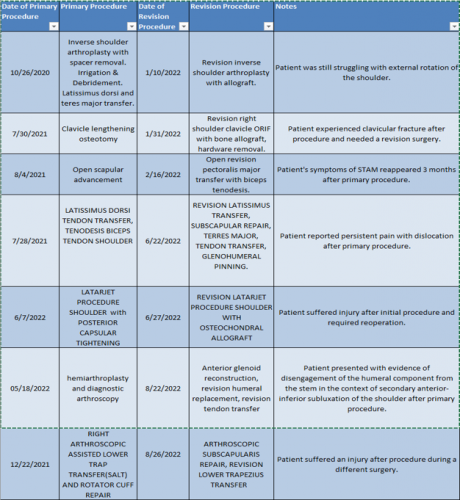
2022 Revision Timeline
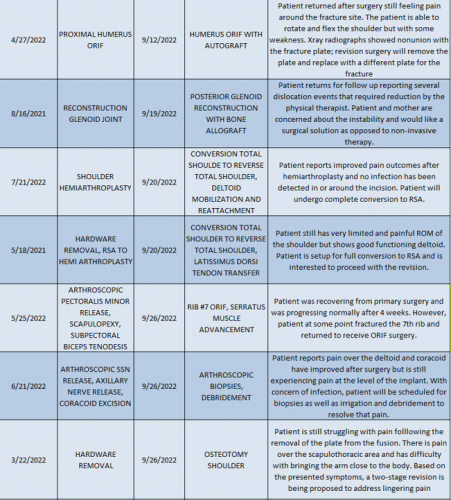
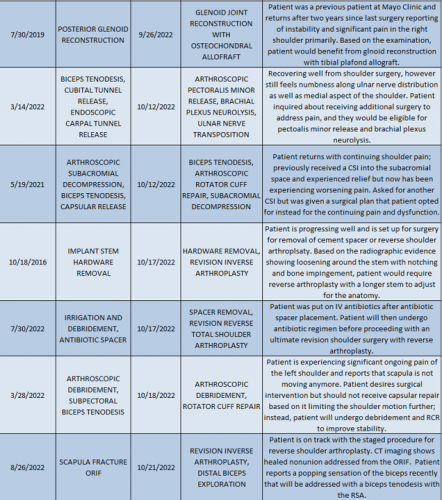
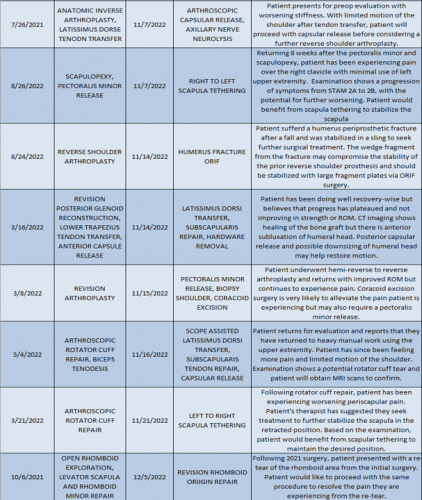
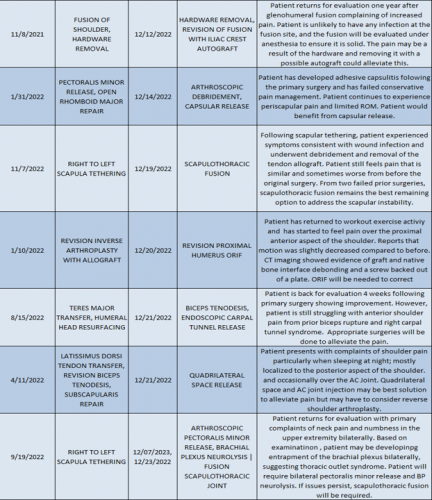
For the 10% of Dr. Elhassan’s cases that required a revision, the average length between the primary (index) and revision procedure was 0.75 years, ranging from 16 days to 5.9 years (yellow portion of the graph above). These revision procedures are summarized below:
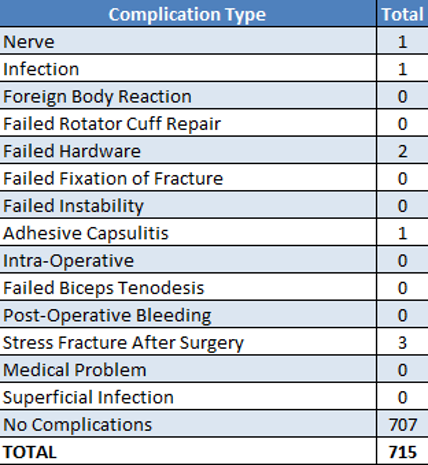
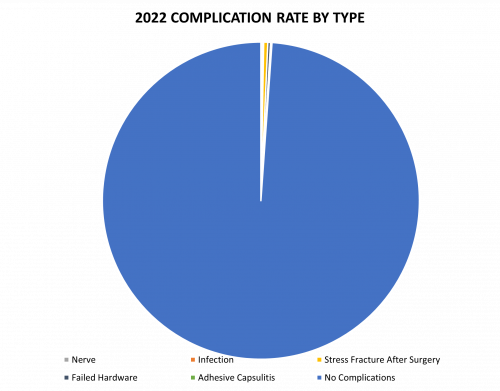
2022 Surgical Complications
Reported below are all of Dr. Elhassan’s complications during the 2022 calendar year. Of the 715 surgeries performed by Dr. Elhassan, 8 patients (1.12%) experienced a complication. These complications were identified in the calendar year 2022, but the primary operation could have occurred in prior years. Please see the data depicted below. Of note, stress fractures after surgery constitute the most prominent complication.
Management of Complications
Of all the 715 surgeries in 2022, 7 cases (1%) had to be readmitted (or expect to be readmitted) to the hospital for an additional operation. In the spirit of transparency and accountability, the Boston Shoulder Institute is providing details for each complication. This will enable patients to be fully informed as to the risks of surgery. Each of Dr. Elhassan’s 2022 complications is detailed below, along with whether it is resolved or ongoing.
Of the 7 total cases, 3 are on their way to recovery and 4 have an ongoing problem. These are shown below in Green (recovered) and Red (not fully recovered).
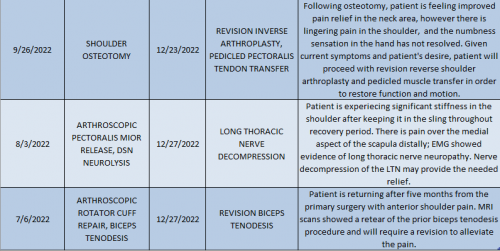
A detailed recount of readmissions follows:
Nerve
Patient returned for evaluation with primary complaints of neck pain and numbness in the upper extremity bilaterally. Based on examination, patient may have been developing entrapment of the brachial plexus bilaterally, suggesting thoracic outlet syndrome. The plan now is for the patient to get a bilateral pectoralis minor release and BP neurolysis. If issues persist, scapulothoracic fusion will be required.
Stress Fracture after Surgery
Patient experienced a clavicular fracture after procedure when reaching for an object. Patient was readmitted shortly after for a revision ORIF of the clavicle with bone allograft and hardware removal. Patient is now doing well and progressing well after therapy and home exercises. The pain is progressively getting better.
After surgery, patient experienced an avulsion of the distal aspect of the coracoid bone transfer. Patient was readmitted for a revision laterjet procedure with osteochondral allograft. Patient still reports having minor pain and catching with her left shoulder, but not enough to merit an intervention.
Patient was recovering from primary surgery and was progressing normally after 4 weeks. However, patient at some point fractured the 7th rib and returned to receive ORIF surgery. Patient is now recovering with physical therapy.
Failed Hardware
Patient returned for evaluation one year after a glenohumeral fusion complaining of increased pain. Patient is unlikely to have any infection at the fusion site, and the fusion will be evaluated under anesthesia to ensure it is solid. The pain may be a result of the hardware and removing it during surgery with a possible autograft could alleviate this.
Infection
Following scapular tethering, patient experienced symptoms consistent with wound infection and underwent debridement and removal of the tendon allograft. Patient still feels pain that is similar and sometimes worse than before the original surgery. From two failed prior surgeries, scapulothoracic fusion remains the best remaining option to address the scapular instability. Final recovery is not yet known.
Adhesive Capsulitis
Patient has developed adhesive capsulitis following the primary surgery and has failed conservative pain management. Patient continues to experience periscapular pain and limited ROM. Patient plans to schedule a capsular release. Patient continues to be followed up for their adhesive capsulitis.
Itemized details for the remaining complication that did not require readmission are as follows:
Failed Hardware
Patient presented with evidence of disengagement of the humeral component from the stem with secondary anterior-inferior subluxation of the shoulder 3 months after primary procedure. Patient then underwent a revision hemiarthroplasty with exchange of humeral head component, glenoid reconstruction with allograft and teres major transfer. During latest visit, patient feels that they have good range of motion of the shoulder but with lingering pain over the anterior aspect of the shoulder. Patient is continuing physical therapy before pursuing further surgery. Final recovery is not yet known.
