Avascular Necrosis (AVN) of the Humeral Head
(David Privitera, M.D.; Paul Yannopoulos, B.A.; Jon JP Warner, M.D.) Dec. 2012
AVN stands for avascular necrosis which is also sometimes referred to as osteonecrosis (osteo= bone; necrosis= dying tissue), which means the bone dies as a result of loss of its blood supply. This can happen due to trauma which results in a fracture or due to other factors which are described below. AVN most commonly affects the hip joint, but it can affect other joints including the shoulder (humeral head) (see below).
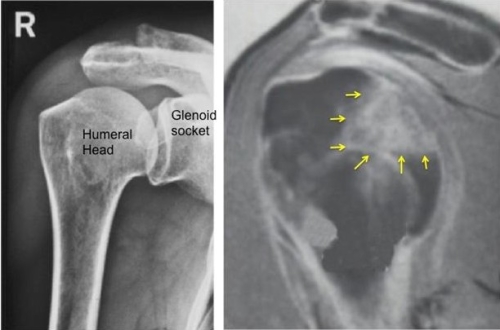
Then normal joint is shown on the left with a round humeral head (ball) on a concave glenoid (socket). With AVN the blood supply to the ball is damaged and a segment of the humeral head may collapse (arrows in images on the right).
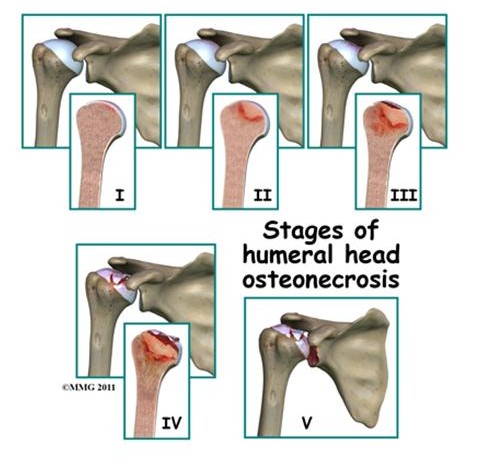
When the blood supply to the ball (humeral head) is lost the bone dies. This by itself is not the main problem, but the body’s healing response results in a series of events which creates the problem. As the bone dies and then blood flow comes back to the bone, the cells in the bone (osteoclasts) remove the dead bone which is then replaced by new healthy bone (osteoblasts). There is an imbalance in this process where dead bone may be removed faster than new bone is created. This results potentially in collapse of the bone as it is weaker than normal. The cartilage which forms the joint may then break down as it looses its support of the underlying bone. (See figure below)
Medical research has identified a number of risk factors associated with AVN. Interestingly, not everyone who has a risk factor gets AVN and not everyone with AVN has an easily identifiable risk factor, meaning the cause is unknown or idiopathic.8
People who have a fracture of the proximal humerus (ball part of the shoulder) are at risk for AVN. With a fracture of the proximal humerus the blood supply can be disrupted and loss of the normal blood flow to the bone may cause it to eventually die and become necrotic. The more extensive the fracture the more likely is this development of AVN. (See figure below)
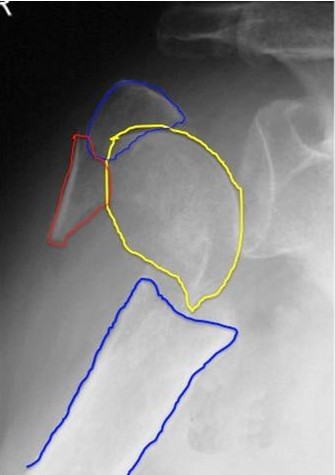
The fracture shown above has resulted in the ball (humeral head- yellow outline) being separated from the other parts of the proximal humerus (Tuberosity shown in red and blue and humeral shaft shown in blue outline).
Another common cause of AVN is the effect of steroids given for other conditions. The steroids are believed to damage the health of the cells which make bone in the humeral head and when they die the sequence of AVN occurs. Other causes of AVN can be radiation or chemotherapy treatment in the case of cancer. Other rare causes include sickle cell disease, Gaucher’s disease, Caisson’s disease (also known as diver’s disease or the bends: This is due to sudden change in water pressure in deep sea diving where nitrogen bubbles form in the blood and damage the blood supply to the humeral head). 1,2,8
In its early stages AVN may not be apparent on a plain x-ray but it can be seen on an MRI (described above). As it progresses with collapse of the humeral head and eventual arthritis it is clearly seen on an x-ray (see figures below).5
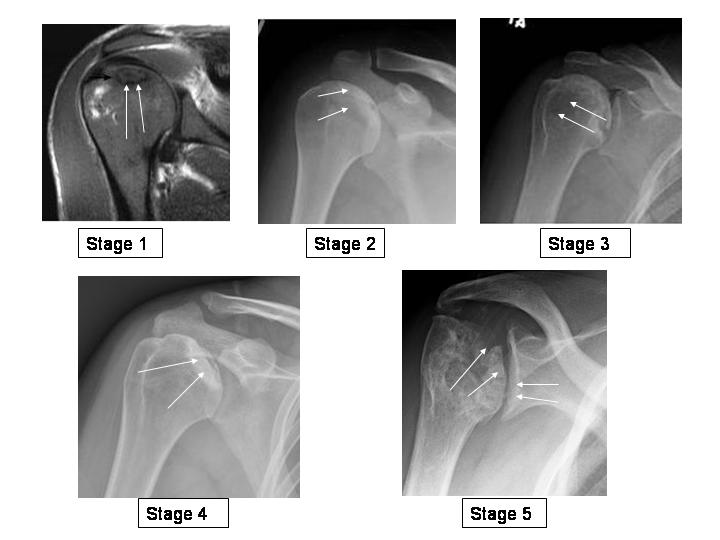
Stage 1 is a shoulder with a normal X-ray but signal changes on MRI showing subchondral edema. Stage 2 is a shoulder with more whitened bone called sclerosis, near the joint surface (subchondral). Stage 3 demonstrates a crescent sign or collapse or fracture of the subchondral bone. Stage 4 demonstrates flattening of the humeral head from advanced collapse. Stage 5 or end-stage AVN demonstrates advanced collapse of the humerus with degenerative changes of the glenoid (arthritis).
 The above picture is an intraoperative X-ray of a percutaneous drilling of AVN of the humeral head.
The above picture is an intraoperative X-ray of a percutaneous drilling of AVN of the humeral head.
Arthroscopy may also be helpful in some cases if the cartilage is damaged and loose pieces in the joint are causing pain. These can be removed with an arthroscopic technique as depicted below.
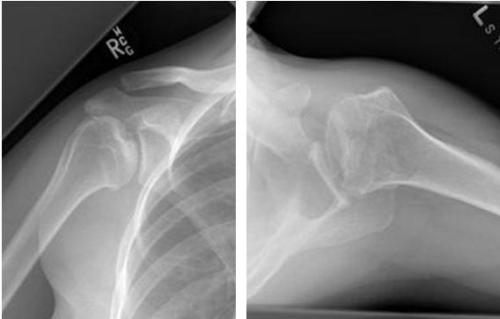
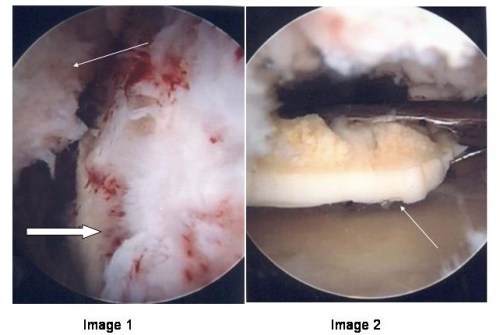
The two X-ray images above show advanced AVN with collapse of the humeral head with areas of fragmentation of the humeral head and mild degenerative changes of the glenoid (socket). The arthroscopic intraoperative picture of this patient, labeled image 1, reveals a view of the humeral head (thick arrow) from inside the shoulder joint. On the humeral head, the cartilage (white) is irregular in appearance with thinning and delamination (peeling off the bone). There is subchondral bone visible (yellow) and a loose body in the field of view (thin arrow). The arthroscopic picture labeled image 2 shows a better look at the loose body (thin arrow). The metal grasper is holding onto the loose osteochondral fragment with the cartilage of the humeral head appearing white and the necrotic bone appearing yellow.
When AVN is more advanced and the humeral head collapse leads to pain, the treatment is similar to arthritis from degenerative disease. Partial replacement of the humeral head (figure) or complete replacement (figure) may be necessary.

The patient above has avascular necrosis involving only part of the humeral head (yellow arrows) shown in the figure on the left. A partial replacement of the humeral head relieved his symptoms and he returned to work as a truck driver.
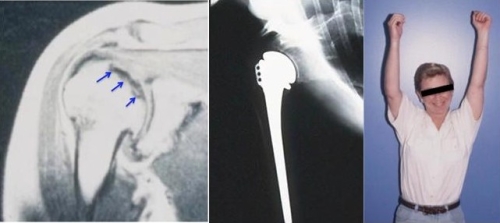
This 42 year old woman developed AVN after a fracture (figure on the left) and underwent a replacement of the humeral head (hemiarthroplasty) as shown in the figure in the middle. Eight years after her surgery she continues to work as a waitress, pictured on the right.
- Mont MA, Payman RK, Laporte DM, Petri M, Jones LC, Hungerford DS: Atraumatic osteonecrosis of the humeral head. J Rheumatol 2000; 27:1766-1773
- Hasan S, Romeo A: Nontraumatic osteonecrosis of the humeral head J Shoulder Elbow Surg 2008; 281-298
- CruessRL: Corticosteroid-induced osteonecrosis of the humeralhead. Orthop Clin North Am 1985; 16:789-796.
- LaPorteDM, MontMA, MohanV, JonesLC, HungerfordDS: Multifocal osteonecrosis. J Rheumatol 1998; 25:1968-1974.
- CruessRL: Experience with steroid-induced avascular necrosis of the shoulder and etiologic considerations regarding osteonecrosis of the hip. Clin Orthop Relat Res 1978; 130:86-93
- HattrupSJ, CofieldRH Osteonecrosis of the humeral head: Relationship of disease stage, extent, and cause to natural history. J Shoulder Elbow Surg 1999; 8:559-564.
- Feeley BT, Fealy S, Dines DM, Warren RF, Craig EV. Hemiarthroplasty and total shoulder arthroplasty for avascular necrosis of the humeral head. J Shoulder Elbow Surg 2008;17(5): 689-694.
- Harreld KL, Marker DR, Wiesler ER, Shafiq B, Mont M. Osteonecrosis of the Humeral Head. J Am Academy of Orthop Surgeons 2009;17(6): 345-355.
