Frozen Shoulder (Adhesive Capsulitis)
(JK Eichinger, M.D., PF Yannopoulos, BA, JJP Warner, MD) Dec. 2012
Frozen shoulder is a term used to describe a shoulder which is stiff. The patient notices loss of motion usually in more than one direction. The medical term for frozen shoulder is “adhesive capsulitis.” This term means that there is an inflammation (capsulitis) that results in tissue becoming thick and adhering to other tissues (adhesive.) [Figure below].Typically a patient will notice pain followed by loss of motion and this may or may not be associated with an injury. The ability to perform daily living activities as well as sports is affected by loss of motion.
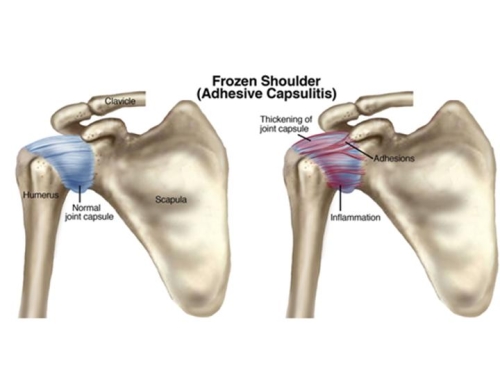
Figure. The normal shoulder joint capsule is loose so that the shoulder can move allowing overhead motion (far left). With the development of adhesive capsulitis, irritation of the lining of the joint leads to scaring and tightening of the capsule (far right).
Normal shoulder motion varies greatly as some “normal” individuals are lax or loose jointed and some are tighter. Both situations are within the range of normal shoulder motion.
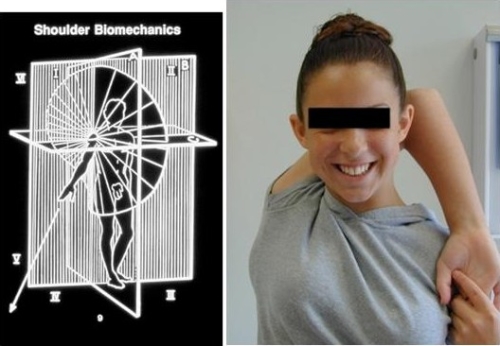
Figure: The normal shoulder mechanics allows for a wide range of motion in multiple directions (left image). The range of normal includes individuals who may be very loose jointed without symptoms (right image)
There are many causes of a frozen shoulder. These can be classified as primary and secondary. Primary causes include idiopathic frozen shoulder (no known cause) and secondary causes include diabetes, trauma, and surgery. The differences are described below. All of these involve some element of inflammation of the joint (synovitis) and this leads to the development of scarring and adhesions so that the joint capsule contracts. The exact cause of this is unclear but appears to be the result of inappropriate cellular activity so that inflammation and healing (scar formation) occurs inappropriately.Women are affected more frequently than are men by a factor of two time, and diabetics have a four times risk of frozen shoulder. If an individual develops a frozen shoulder on one side they are at risk for a similar problem on the other side. (Neviaser, JBJS, 1945; Hsu, JSES, 2011)

In a normal shoulder (image on left) the ligaments and capsule appear white and thin. With a frozen shoulder (image on right) the capsular lining (synovium) appears red as the result of inflammation, and the joint capsule appears thickened.
In the case of a primary frozen shoulder (idiopathic adhesive capsulitis) three phases have been described. These include Stage 1 which is called the “freezing” stage; Stage 2, the “frozen” stage; and Stage 3, the “thawing” phase. Stage 1 is usually characterized by pain, which proceeds loss of motion. Stage 2 is accompanied by loss of motion. And stage 3 is characterized by gradual improvement of motion. (See figure below). The time course for all three stages can range from four to 20 months; however, the distinct phases may overlap and not be so clear in some patients. Indeed, some patients may continue to have marked pain even as they become stiff, and this may be related to the loss of motion causing irritation of the surrounding structures including the rotator cuff.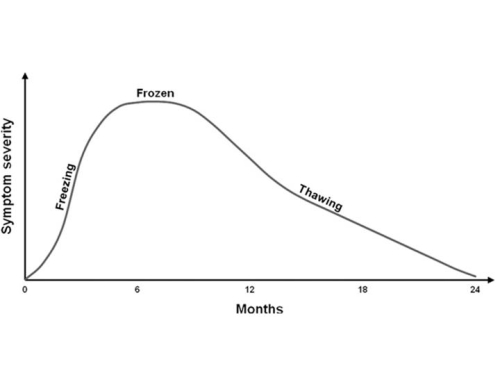
Figure 2. Continuum of Phases in Adhesive Capsulitis. Hsu, et al. Current review of Adhesive Capsulitis. JSES, 20;502-514, 2011.
The diagnosis of frozen shoulder can often be difficult to make and may be missed by a physician who thinks the patient’s problem is related to a rotator cuff problem or tendonitis. A typical patient who presents with the idiopathic (primary) form is a woman who notes the onset of pain, perhaps after a minor trauma or even no trauma. Then loss of motion follows. Sometimes surgery is recommended for tendonitis or a rotator cuff tear. The problem with this approach is that aggravate the frozen shoulder in some patients.The patient presents with motion loss, which is usually painful. (Figure below). In most cases it is advisable to obtain an x-ray to make sure the motion loss is not due to arthritis.

Fig. Loss of flexion is demonstrated in a 42-year-old woman with diabetes (left image) and loss of external rotation is shown in a 21-year-old woman after an arthroscopic repair of shoulder instability (right image).
There are different factors, which contribute to a frozen shoulder,. In the case of a primary (idiopathic) frozen shoulder the capsule is shortened and thickened (see figure below).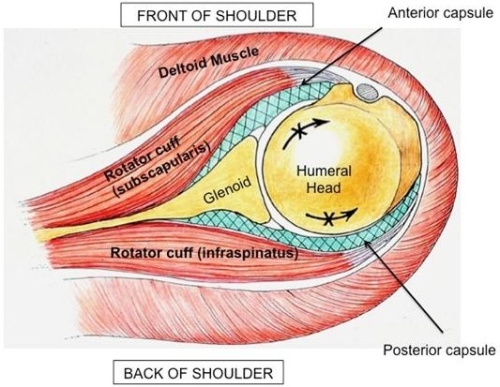
Fig. In adhesive capsulitis the capsule is shortened, thickened and scarred (green cross-hatched layer); however, all of the rest of the shoulder is normal.
In the case of post-traumatic frozen shoulder, which may occur after a fracture, the extent of scarring may involve not only the capsule but also the tissue planes, which can scar to each other. This is particularly the case after a fracture repair of the shoulder.
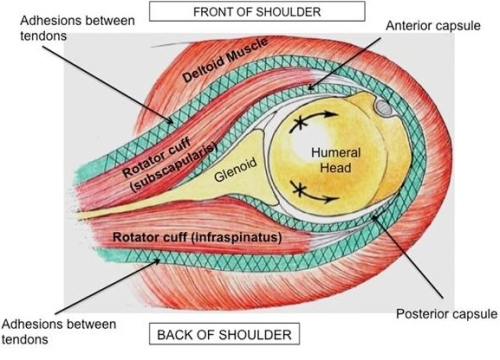
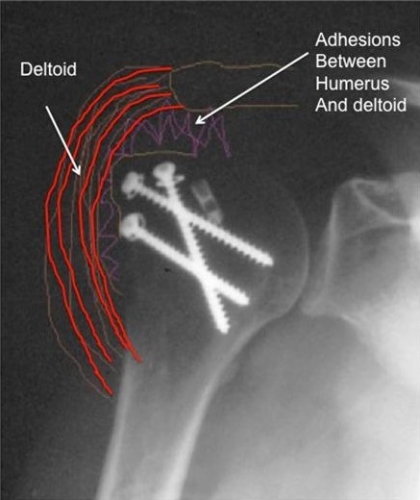
Upper Figure: In the case of post-traumatic frozen shoulder there are adhesions which involve not only a shortened, scarred capsule (green cross-hatched area) but also scarring and adhesions between the tissue planes in the shoulder (green cross-hatched area).
Lower Figure: After a fracture repair in which surgery is performed to place screws and sometimes a plate, adhesions may develop between the deltoid and the humerus.
In the case of stiffness after instability surgery, the ligament and capsule in the front of the shoulder may be tightened so as to mainly limit the patient’s external rotation (arm out to the side). In a worst-case scenario, the tight anterior shoulder structures may push the humeral head (ball) out the back of the shoulder and lead to arthritis. (Figure below).
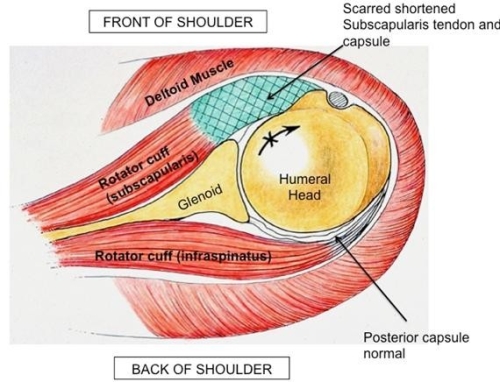
Fig. An open instability surgery may result in tightening of the capsule and ligaments as well as the subscapularis tendon in the front of the shoulder.

Fig. Loss of external rotation in a young man after an instability surgery.
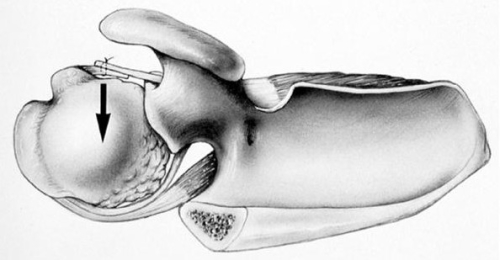
Upper figure: Over-tightening of the ligaments in the front of the shoulder forces the humeral head out the back of the joint resulting in joint overload and development of arthritis.
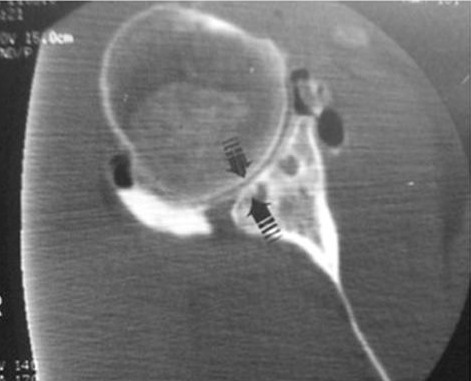
Lower figure: This CT scan demonstrates the development of arthritis with loss of joint space in the back of the shoulder (arrows) after instability surgery.
Non-operative:
In the case of primary frozen shoulder (idiopathic) the majority of patients will get better with either no therapy or with a supervised physical therapy program of gentle stretching (Vastamämaki et al,CORR 2012; Hand C et al, JSES 2008; Diercks and Stevens, JSES 2004; Kavimäki et al, JSES 2007; Levine et al, JSES 2007).
In patients with severe pain and mild loss of motion, injection of cortisone into the joint may provide dramatic relief and possible shorten the time course for recovery (Griesser et al, JBJS 2011; Favejjee et al, 2011- check pubmed.org; Blanchart V et al, Physiotherapy; Lorbach et al, JSES 2010; Jacobs et al, JSES 2009; Marx et al, HSS 2007
In the rare cases of chronic stiffness, which is refractory to a conservative approach, operative intervention is a reasonable approach. While such surgery is necessary only rarely with primary (idiopathic) frozen shoulder secondary (post-surgical and post-traumatic) frozen shoulder are usually more resistant to conservative treatment. (El Hassan et al, JSES 2010)
A specific consideration is stiffness after rotator cuff surgery, which has an estimated incidence of only 4% (Huberty et al, Arthroscopy 2009). In most patients stiffness after rotator cuff repair is not a cause for alarm as it usually resolves within the year after surgery and it may be associated with a higher healing rate of the repair.
In the case of stiffness after instability surgery, there can be cause for concern. Untreated loss of external rotation may contribute to the development of arthritis after a period (see above figure.). Thus, when therapy is ineffective surgical release of the stiff joint capsule is an important consideration.
In the case of stiffness after a fracture repair, adhesions may be extensive and involve not only the joint capsule but also the tissue planes (See figure above). This can also lead to refractory stiffness, which requires surgical intervention.
Surgical Options:
Manipulation under anesthesia:
Historically, this has been the preferred approach of many surgeons. (Vastamäki et al, CORR 2012; Jenkens et al, JSES 2012; Thomas et al, JBJS 2011; Jacobs et al, JSES 2009; Farrell et al, JSES 2005) This method involves manipulation of the shoulder under anesthesia in order to disrupt adhesions and restore motion. While it has been shown to be effective, complications such as fracture, nerve injury and dislocation have been described. Patients with diabetes have also been shown to be at greater risk for recurrence of stiffness after manipulation (Jenkens et al, JSES 2012) Arthroscopic techniques to release the capsule prior to manipulation of the shoulder have been described as an alternative more recently. (Rill et al, AJSM 2011)
Arthroscopic Capsular Release:
Arthroscopic capsular release was first introduced as a surgical option in the late 1990’s (Warner et al, JBJS 1996; Ticker et al, Arthroscopy 2000). Since then it has become a commonly employed method shown to be very effective with a durable outcome of restoring shoulder motion to normal (Le Lievre and Murrell, JBJS 2012; ELHassan et al, JSES 2010).
Our approach:
Anesthesia during surgery and pain control after the arthroscopic release of the stiff shoulder are very important. In some cases we prefer to use an interscalene nerve block in order to control pain for 24-48 hours after surgery (see figure below). This is a catheter placed adjacent to the nerves in the neck, which control sensation, and pain in the shoulder. This method can be very effective for pain control, which allows immediate physical therapy to maintain flexibility of the shoulder after surgery.

The arthroscopic release of adhesions and the capsular contracture is performed using a arthroscopic which is a thin tube that is inserted into the shoulder joint and provides a view of the inside of the capsular contracture. Special instruments are then used to release the adhesions (see figures below)
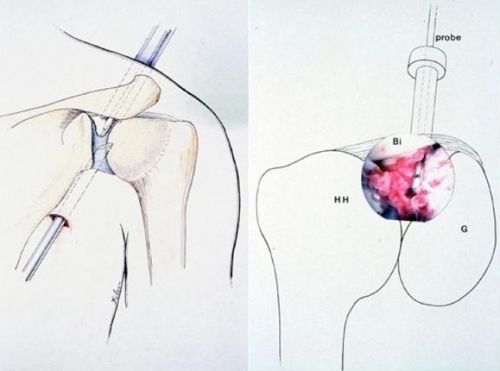
The arthroscope is inserted from the back of the shoulder and the tight capsule in the front of the upper portion of the joint is release as the first step (figure on left). The capsule may appear to be red and thickened due to inflammation (figure on right) The humeral head (HH), glenoid socket (G), biceps (Bi) and probe are labeled (figure on right).
Click this link to view the video
This video demonstrates release of the thick, scarred capsule in the front of the shoulder. The normal capsule is only a few millimeters thick. Here the capsule is about 10mm thick.
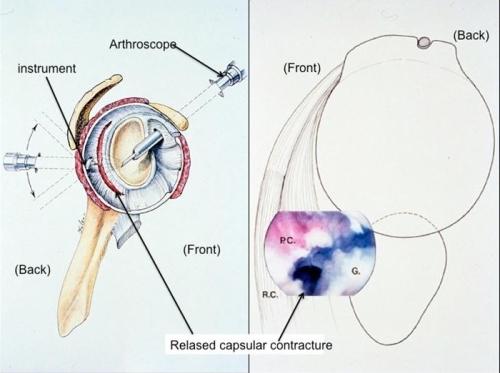
Figure: The posterior capsule is also released. The image on the left demonstrates the placement of the arthroscope and the instrument, which releases the capsule in the back of the shoulder. The image on the right shows the actual release of the stiff capsule in the back of the shoulder (P.C.). The glenoid socket (G) and rotator cuff (R.C.) are also labeled.
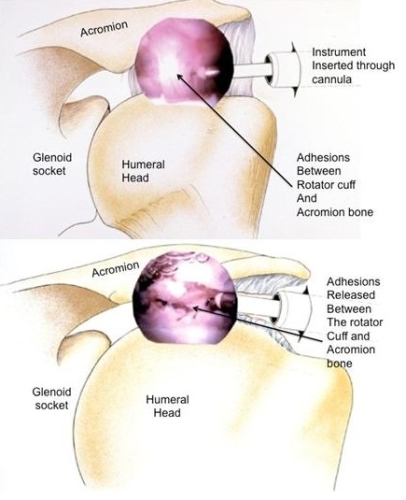
FIGURE: Adhesions may develop between the rotator cuff and the acromion bone. This may occur after rotator cuff surgery or other shoulder surgery. This is outside the joint and may be released effectively using and arthroscopic technique.
What do I do after surgery?
In some cases the patient remains in the hospital for 24-48 hours so that the interscalene pain catheter can provide pain relief. During this time the patient will be treated by the physical therapist with stretching exercises twice a day, in the morning and the afternoon. Upon discharge, the patient is instructed to remove the sling and begin stretching at home and using the arm for all daily living activities. Physical therapy after surgery will be individualized depending on each patient’s needs.
(Physical therapy exercises described in the tab below.)
Open Surgical Release:
In patients where the extent of adhesions is too significant for an arthroscopic approach, or the tendons outside the shoulder have been scarred, an open surgical release is required. The steps involve and incision and release of the adhesions between tissue planes, and sometimes lengthening of tendons (See figures below).
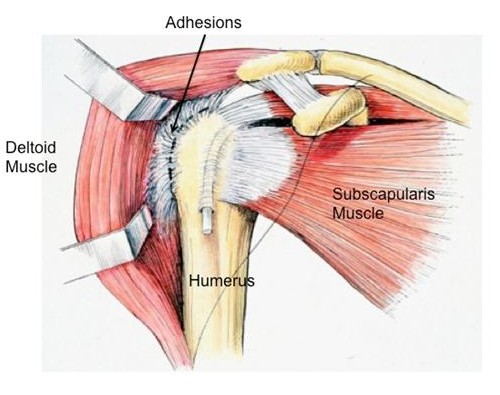
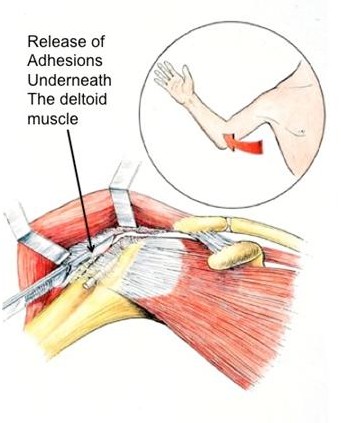
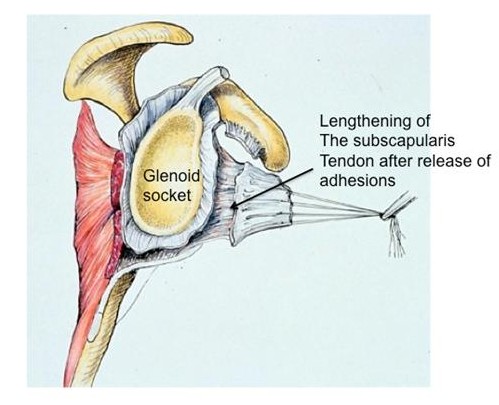
Figures: An open approach allows for release of adhesions between the tissues and also lengthening of the tendons, which may be shortened. This cannot be so effectively done arthroscopically.
Results:

Figure: This patient has chronic stiffness with loss of external rotation with the arm at the side (left image) and with the arm abducted out to the side (right image).
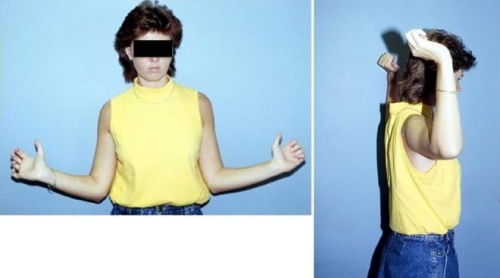
Figure: Six months after an arthroscopic release the patient has regained normal external rotation with the arm at the side (left image) and abducted out to the side (right image).

This patient has loss of external rotation as the result of over-tightening of the shoulder with an instability surgery.

Figure: One year after surgery the patient has near normal external rotation with the arm at the side (image on right) and abducted out to the side (image on left).
Overall results with arthroscopic and open release are excellent; however, the extent of scaring and damage from prior surgery may influence the outcome.
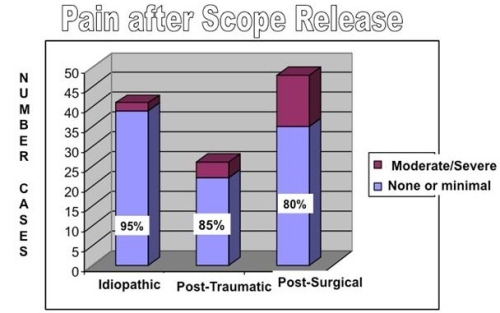
Figure: This figure shows the number of cases over a 10-year period operated by Dr. Warner for frozen shoulder.
The pain relief after surgery is best in patients with primary (idiopathic) frozen shoulder and less reliable but good in patients who have stiffness in secondary (after trauma or after surgery) frozen shoulder.
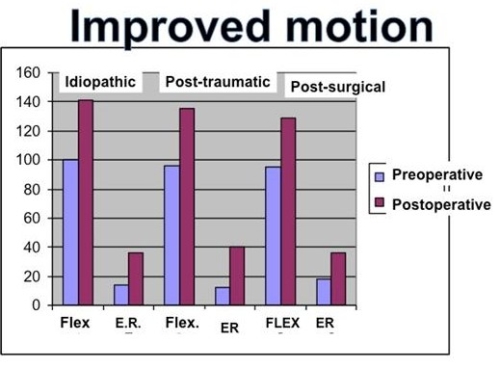
Figure: This graph shows the gain in motion from preoperative (blue) to postoperative (red) following arthroscopic release for frozen shoulder. Primary (idiopathic) gains more motion than do the other conditions. Flex = Flexion; E.R. = External Rotation.
Jon JP Warner, MD. Frozen Shoulder: Diagnosis and Management. J Am Acad Orthop Surg 1997;5:130-140.
-Outlines diagnosis and modern treatment techniques
-Original description of the condition of frozen shoulder
Warner JJ, Allen A, Marks PH, Wong P. Arthroscopic release for chronic, refractory adhesive capsulitis of the shoulder. J Bone Joint Surg Am 1996;78:1808-16.
-Original study describing arthroscopic treatment of adhesive capsulitis
-Arthroscopic surgery is effective for many forms of shoulder stiffness including primary adhesive capsulitis
– This follow-up study revealed that patients without surgery compared to patients with surgery have equivalent outcomes.
-Most patients will do well over the long term with no treatment but up to 35% will have some loss of motion. 6% will have a poor outcome.
-Patients with idiopathic frozen shoulder were examined prospectively to two treatment options compare “Supervised neglect” or patient directed therapy within the limit of pain to that of intensive physical therapy. Supervised neglect yielded superior results both in terms of motion and pain relief.
-A randomized, prospective study evaluating two treatment groups: home exercise alone and manipulation under anesthesia with home exercise. Both groups had equivalent outcomes in motion and pain after one year of follow-up.
-A systematic review of studies evaluating the effectiveness of intra-articular cortisone injections for adhesive capsulitis. Intra-articular cortisone injections and oral steroids appear to improve pain in the short term but no definitive difference could be determined at long-term follow-up.
-A review of 6 prior studies comparing physical therapy and intra-articular cortisone injections with findings that cortisone injections in the short term improve symptoms but in the long term there is minimal difference between the two treatment groups.
-A prospective randomized trial comparing oral steroids and 3 consecutive intra-articular cortisone injections at 0, 4 and 8 weeks. The patients receiving cortisone injections had better range of motion and patient satisfaction than patients who received oral steroids. Both groups had similar pain scores.
-A prospective study evaluating two treatments consisting of manipulation under anesthesia or three consecutive cortisone injections at 0, 6 and 12 weeks. At two years the authors reported equivalent outcomes in terms of range of motion and pain relief.
-A retrospective evaluation of intra-articular cortisone injection for Stage I and Stage II adhesive capsulitis revealed that an early cortisone injection for patients in Stage I can effect resolution in an average of 6 weeks and or patients in Stage II at an average of 7 months.
-In a series of 489 consecutive arthroscopic rotator cuff repairs, 24 patients (4.9%) developed postoperative stiffness. Risk factors for postoperative stiffness were calcific tendinitis, adhesive capsulitis, single-tendon cuff repair, PASTA repair, being under 50 years of age, and having Workers’ Compensation insurance. Twenty-three of 24 patients (95.8%) showed complete healing of the rotator cuff. Arthroscopic release resulted in normal motion in all cases.
-Diabetic patients treated with manipulation under anesthesia sustained a 36% recurrent rate requiring a second manipulation.
-A prospective, randomized clinical trial comparing manipulation under anesthesia and cortisone injection. There were no clinical outcome differences between the two groups suggesting that injection was as efficacious and safer than manipulation under anesthesia.
-Long term follow-up on a cohort of patients treated with manipulation under anesthesia showing maintenance of motion at 15 years.
-Patients with residual motion deficits still have high patient satisfaction in follow-up after both operative and non-operative treatment.
-This article describes the recognition and successful arthroscopic treatment of posterior capsular contracture in a retrospective evaluation of a cohort of patients.
-Long term follow-up on a cohort of 43 patients treated with a 360-degree arthroscopic capsular release. At an average follow-up of 7 years, patients maintained marked improvement in pain, range of motion and patient satisfaction.
