Dr. Warner’s Surgical Outcomes Report: 2018
Dr. Warner’s outcomes data was systematically reviewed by his two Research Assistants utilizing the medical records system of Massachusetts General Hospital. This involved review of Dr. Warner’s operations on a case-by-case basis, with special consideration made to procedure type, patient past surgical history to determine primary or revision status, and any complications arising from the operation. This data was collected, aggregated, and analyzed by the two Research Assistants with no outside influence from the attending physician.
Physician Overview for the Year 2018
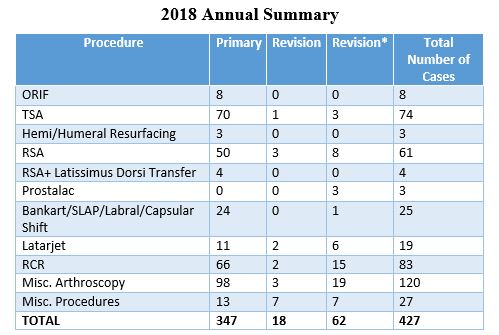
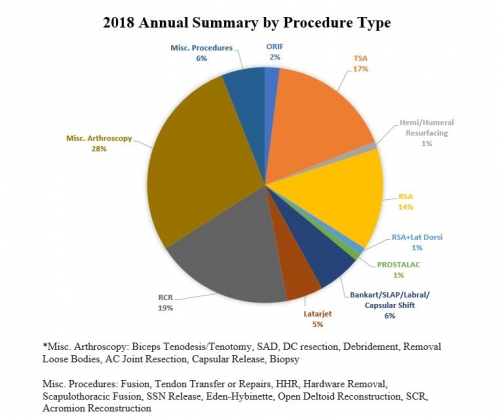
- Dr. Warner performed 427 surgeries throughout the year 2018.
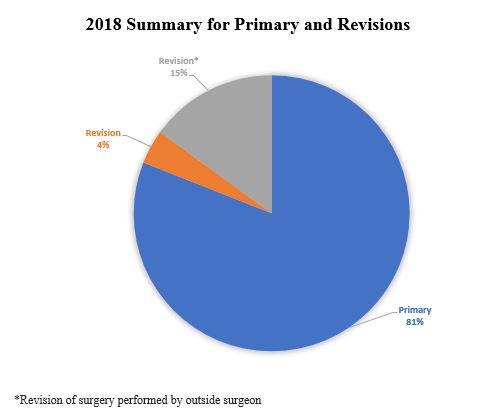
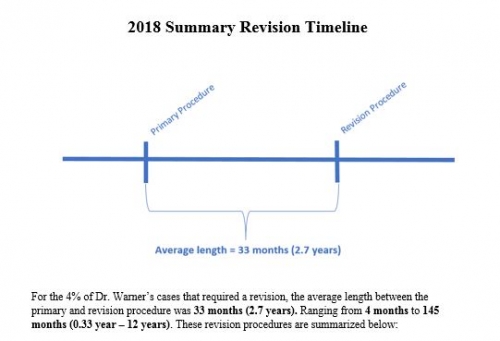
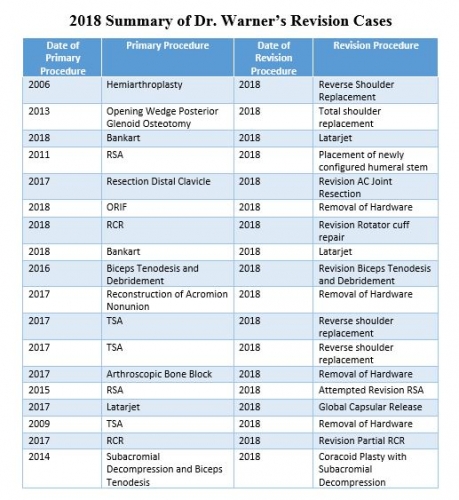
- Of the 427 operations, 18 were revisions of his own cases, 62* were revisions of other surgeons’ cases, and 347 were primary surgeries (Of note, Dr. Warner’s revisions were performed in the 2018 calendar year, but the primary operation could be from prior years).
-
Dr. Warner’s 2018 surgeries are organized by type below:
2018 Surgical Outcomes Report: Complications
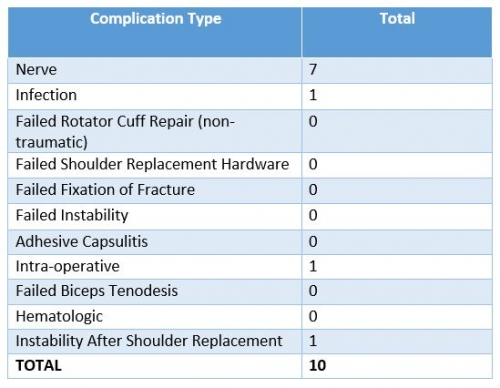
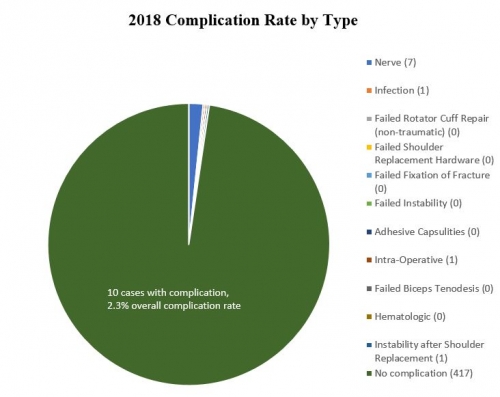
Reported below are all of Dr. Warner’s complications during the 2018 calendar year. Of the 427 surgeries performed by Dr. Warner, 10 patients (2.3%) experienced a complication. These complications were identified in calendar year 2018, but the primary operation could have occurred in prior years. Please see the data depicted below. Of note, nerve injuries constitute the most prominent complication, but 6 out of 7 nerve problems completely resolved and were thus transient stretch injuries.
Management of Complications
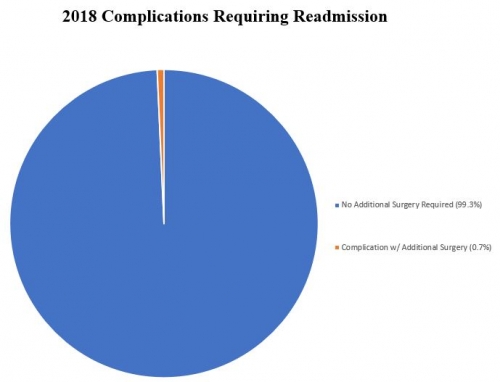
How Many Surgeries Required Readmission?
Of all 427 surgeries in 2018, 3 cases (0.7%) had to be readmitted to the hospital for management. One was for ulnar nerve dysfunction after a Reverse Total Shoulder procedure that was resolved after an ulnar nerve transposition surgery. The second was for a patient who underwent PROSTALAC insertion for an infection after a Hemiarthroplasty. The third was a closed reduction of a Reverse Shoulder Arthroplasty to treat dislocation 2 months following implantation of the prosthesis. Itemized details by case are found in the “Complications by Type” section.
Complication Details by Type
In the spirit of transparency and accountability, the BSI is moving to provide the most detail possible for each complication. This will enable patients to be fully informed as to risks of surgery. Each of Dr. Warner’s 2018 complications is detailed below, along with whether it is resolved or ongoing. The complications are itemized by type:
Intra-Operative (1)
Total Shoulder Arthroplasty – At the time of the immediate postoperative X-ray, it was determined that the humeral head was dislocated anteriorly. Before the patient was awakened, the incision was re-opened, the humeral head was reduced into the glenoid, and the inferior portion of the subscapularis was repaired. RESOLVED.
Nerve Injury (7)
Prostalac – Reported numbness and inability to use left hand two days following surgery. Diagnosed with brachial plexus palsy, which was confirmed via EMG and treated with physical therapy. RESOLVED.
Reverse Shoulder Arthroplasty – Experienced numbness, weakness, and pain in right hand 6 weeks following surgery. Diagnosed with ulnar nerve dysfunction and underwent a transposition of the ulnar nerve approximately 4 months following primary surgery. RESOLVED.
Total Shoulder Arthroplasty – Noted deltoid weakness at 6 weeks post-surgery with suspected axillary nerve neuropraxia. Patient worked with physical therapy on range of motion and strengthening with significant improvement. RESOLVED.
Latarjet – Reported deltoid weakness and numbness through the axillary at 2 weeks post-surgery. Diagnosed with suspected axillary nerve neuropraxia, which was resolved through physical therapy. RESOLVED.
Reverse Shoulder Arthroplasty – Experienced deltoid weakness at 6 weeks post-surgery and was diagnosed with neuropraxia of the axillary nerve following EMG study. Resolved through physical therapy focusing on strengthening and stretching. RESOLVED.
Latarjet – Experienced decreased sensation over the axillary nerve and weak deltoid contraction 6 weeks post-surgery. Patient was diagnosed with a stretch to the axillary nerve, which was subsequently treated with physical therapy. RESOLVED.
Reverse Shoulder Arthroplasty – Patient diagnosed with axillary nerve neuropraxia 2.5 months post-surgery. Awaiting EMG study to confirm the diagnosis, but patient is currently being treated with physical therapy. Follow-up too short to determine resolution. ONGOING.
Infection (1)
Hemiarthroplasty – Patient experienced ongoing stiffness and pain 5 months following surgery performed by Dr. Warner at an outside hospital. Cultures from shoulder biopsy confirmed P. acnes infection, which was treated with PROSTALAC antibiotic spacer insertion 8 months following primary surgery. Biopsies taken 3 months following this operation confirmed clearance of infection, and patient received a reverse shoulder arthroplasty following PROSTALAC removal. Because the complication of infection required additional surgery, the outcome has yet to be determined. ONGOING.
Instability after Shoulder Replacement (1)
Reverse Shoulder Arthroplasty – Patient experienced shoulder dislocation 2 months following reverse shoulder arthroplasty for proximal humerus nonunion. Following a closed reduction of the prosthesis, patient continued to dislocate. A revision treatment plan has been formulated, but patient is awaiting medical clearance before proceeding. Because treatment is pending, it is too early to determine the ultimate outcome of this complication. ONGOING.
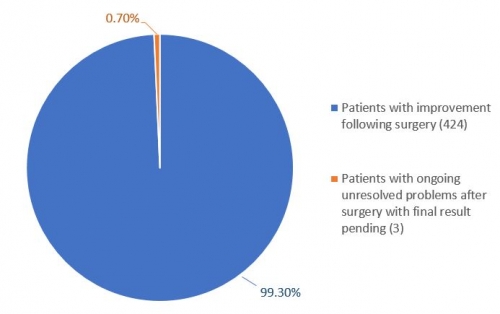
On the whole, only 3 patients of 427 operations have ongoing unresolved problems after surgery with the final result pending.