Instability
The normal Shoulder is composed not only of the glenohumeral joint (“Ball-in-Socket”) but also the the articulation of the scapula with the chest wall (“scapulothoracic articulation”), the connection between the scapula and the clavicle (“AC Joint”) and clavicle to the sternum (“breast bone”) (Fig. 1). Normal shoulder motion means that the scapulothoracic joint must move as well as the glenohumeral joint (Fig. 2). During this motion the glenohumeral joint moves with the humeral head rotating in the glenoid socket (Fig. 3). Use of the arm over the head as in work or sports puts stress on the ligaments which keep the ball in the socket. The normal humeral head (ball) is larger than the glenoid (socket). This anatomy which is similar to a golf ball sitting on a tee, allows for the large range of motion required for throwing a ball as well as reaching behind the back (Fig. 4).
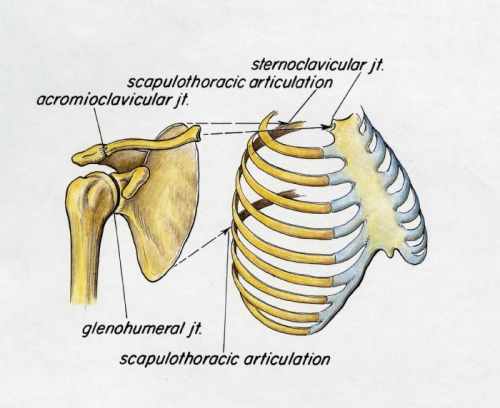
Fig. 1: Shoulder Girdle Complex
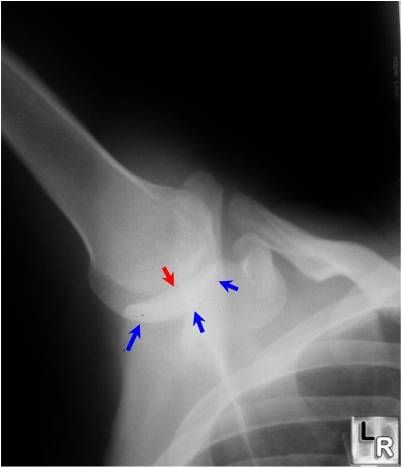
Fig. 2a: The humeral head (ball) remains centered (red arrows) in the socket (blue arrows) if the scapula moves in proper rhythm with the glenohumeral joint motion.
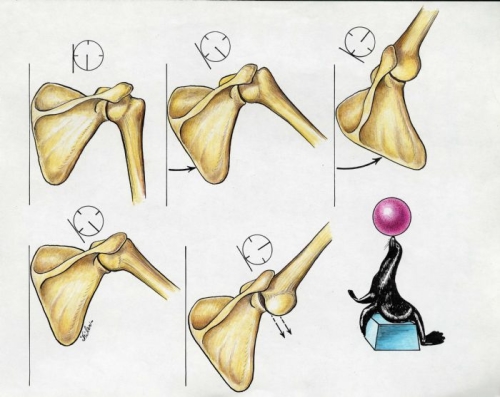
Fig. 2b: Normal scapulothoracic motion allows the scapula to rotate upward so the glenoid (socket) remains underneath the humeral head (Top row). This is similar to a seal balancing a ball on its nose by properly moving its body underneath the ball. If the scapulothoracic motion is not normal and lags behind the glenohumeral motion, the socket may not move into a stable platform position underneath the humeral head and instability can occur as the ball slips out of the socket (lower row).
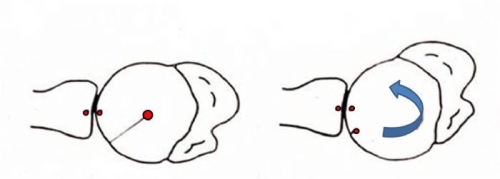
Fig. 3: Normal shoulder rotation is like a ball-in-socket. The humeral head (ball) rotates (arrow) on the socket, but remains centered on the socket (red circles).
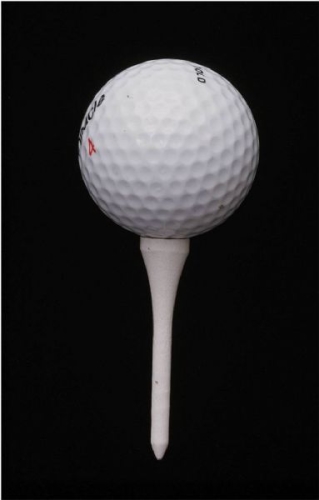
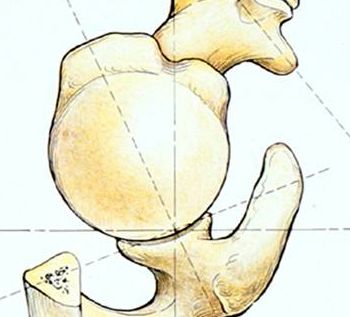
Fig. 4: The ball is bigger than the socket, which allows for the large range of motion in the shoulder. Only 1/3 of the joint surface fo the ball contacts the socket at any time.
The socket is made broader (wider) and deeper by a flexible rim of cartilage (labrum) which runs along its perimeter. This increases stability by making the socket larger and deeper (Fig. 5). The labrum also acts as an anchoring point for the ligaments which stabilize the shoulder joint during shoulder motion.
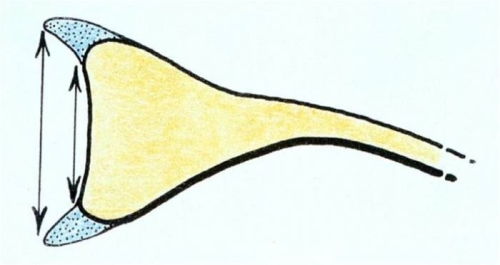
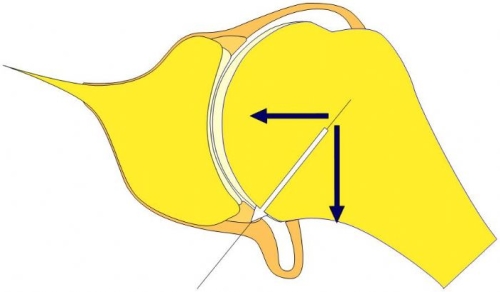
Fig. 5: The labrum broadens and makes deeper the glenoid socket (top image). The labrum also acts as an anchoring point for the ligaments of the shoulder (lower image).
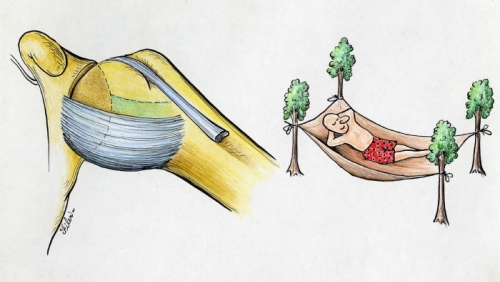
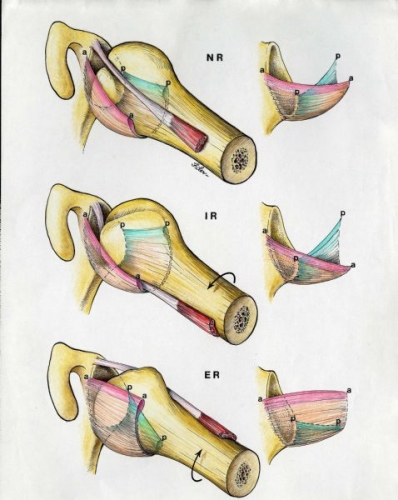
The normal main ligament of the shoulder (inferior glenohumeral ligament) supports the humeral head like a hammock supports a person (top image). With arm rotation, the ligament (hammock) moves forward and backward to keep the ball in the socket during this rotation (lower image).
The role of the (glenohumeral) ligaments are to act like seat belts and airbags of the shoulder limiting extreme rotations and translations of the ball out of the socket (Fig. 6). Much of the stability during normal motion is through compression of the ball into the socket by the rotator cuff muscles. The ligaments provide static stability as they passively limit motion extremes, while the rotator cuff muscles provide dynamic stability by contracting and pushing the ball and socket together (Fig. 7).
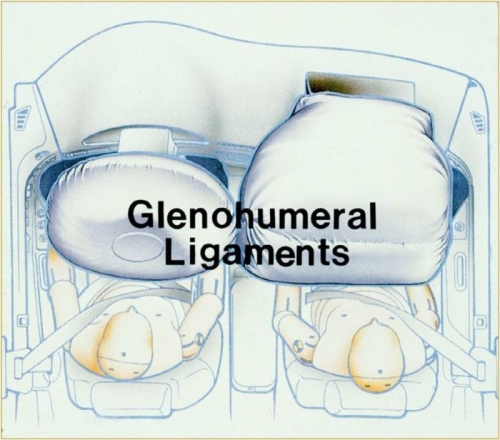
Fig. 6
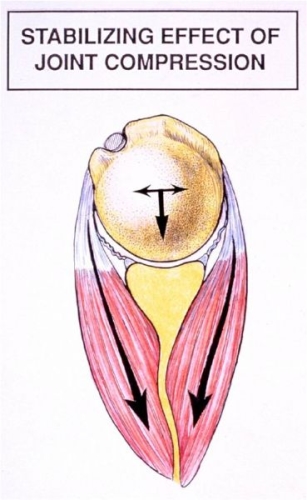
Fig. 7
Normal motion is quite variable as some individuals are loose jointed or lax, but don’t have shoulder instability; and others are relatively tight jointed and have less mobility of the joint (Fig. 8).

Fig. 8A: This individual is hyper-lax, but has no instability.
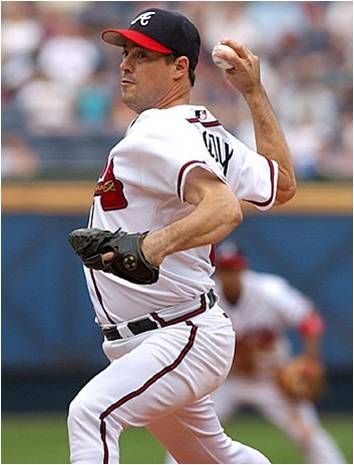
Fig. 8B: A pitcher has increased laxity that allows him to throw a fastball, but his normal ligaments and muscles prevent instability.
Shoulder instability occurs when the humeral head (ball) moves out of the glenoid (socket) during shoulder motion. This is associated with symptoms which are typically pain and sometimes a sense of shifting. If the ball completely moves out of the socket, this is called a dislocation. If the ball moves partially out of the socket, this is called a subluxation. Shoulder instability may occur as the result of a traumatic event such as a football tackle or a fall. It can also occur as a consequence of repeated motions which stretch the ligaments in the shoulder allowing the ball to then move partially out of the socket. While laxity or looseness of the shoulder is a normal attribute of shoulder function, some individuals are at greater risk of shoulder instability due to their normal shoulder joint laxity. Other individuals may have an ability to voluntarily make their shoulder subluxate or dislocate by selectively contracting muscles around the shoulder. These rare individuals do not usually have painful symptoms. Some individuals may have an under-development of the socket which is a congenital (from birth) failure of the socket to form with its normal shape and depth (Fig. 9). This is a rare condition and may not present an individual is in his(her) 20’s or 30’s. Shoulder instability is usually in the anterior (out the front) direction, though in about 10% of individuals it may be posterior (out the back). In another 5-10% of cases shoulder instability may occur in more than one direction. This is called multidirectional instability.
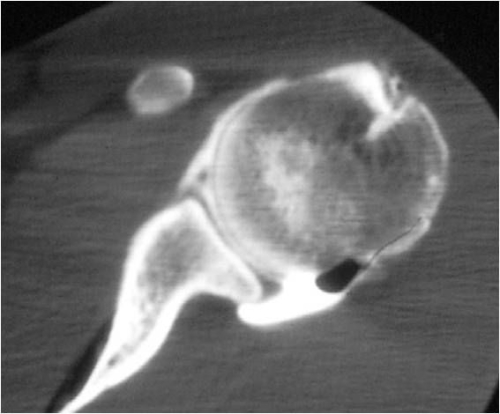
Fig. 9A: Normal shoulder ball-in-socket

Fig. 9B: The socket is dysplastic as the posterior (back) portion of the socket is not completely developed
Most shoulder instability occurs as the result of a sudden and unpredictable traumatic event such as a fall or a collision in sports (Fig 10.). The arm is often out to the side, but some individuals may not recollect the exact position of the arm. When this occurs, the individual may feel the shoulder actually come out of joint or they may just have pain. It is not uncommon for there to be a sensation of a “dead arm” where the individual notes loss of feeling and control of the arm. The shoulder may come completely out of the joint (a dislocation) or it may move partially out of the joint (a subluxation). Sometimes, the ball can move back into the socket on its own, or the individual may find they can get the ball to move back in place by manipulating the shoulder. If the shoulder remains dislocated, it is necessary for the individual to go to an emergency room in order to have a physician reduce the shoulder back into place. This is usually done with intravenous sedation (medicine by vein) so the muscles will relax and with gentle manipulation the arm ball can be reduced back into the socket (Fig. 11).


Fig. 10: Anterior shoulder dislocation usually occurs with a sudden unpredictable trauma, such as a collision, contact, or falling injury.
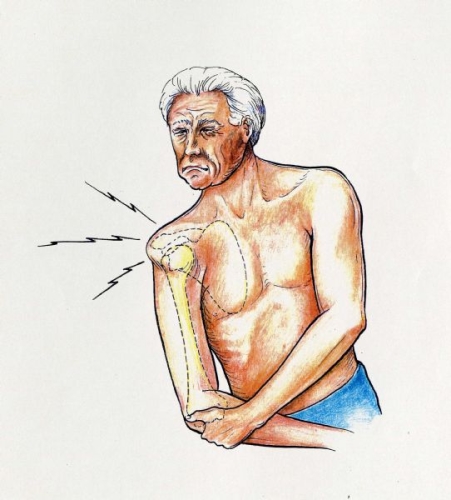
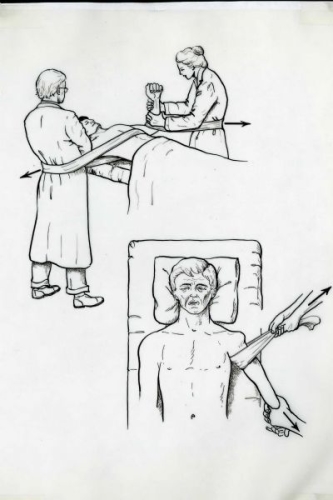
Fig. 11: The shoulder dislocation is usually reduced by some method where the physician gently pulls traction on the arm. Relaxation and pain relief is achieved by intravenous (by vein) administration of medications.
When sufficient force is applied to the shoulder and a dislocation occurs one or more injuries must occur to the ligaments, cartilage, and labrum in the shoulder. The most common injury is called a “Bankart lesion” (named after the surgeon who first described this injury in the 1920’s). This is a separation of the labrum from the edge of the socket (Figure 12). The effect of this injury is to detach the anchoring point of the main (inferior) glenohumeral ligament. This would be analogous to the failure of the attachment point of a hammock to a tree (Fig. 13). In addition the labrum effect which deepens the socket is lost as well (Fig. 14). In some cases the ligament itself can stretch in isolation or in combination with a Bankart lesion. (Fig. 11). Finally the ligament may actually tear in its midsubstance (Fig. 15).
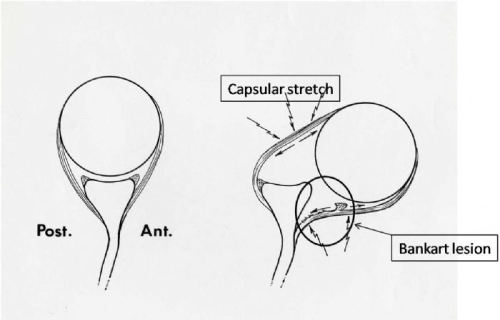
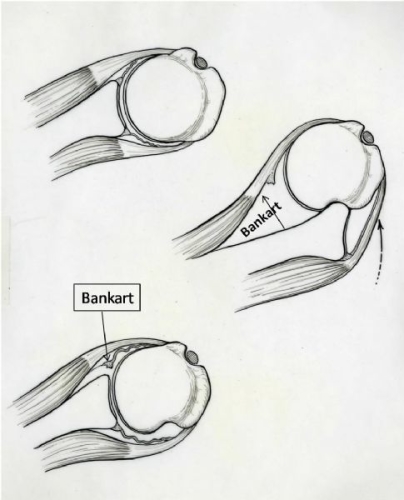
Fig. 12: With an anterior (out the front) dislocation, the most common injury is a Bankart lesion. The capsule may also be stretched.
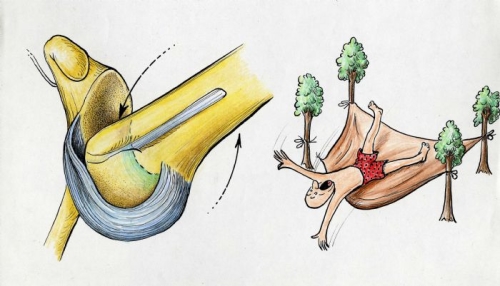
Fig. 13: Injury to the inferior glenohumeral ligament with an anterior dislocation is similar to a hammock failing by either pulling off its attachment or stretching out
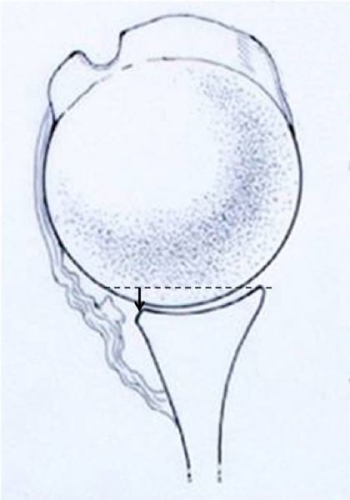
Fig. 14: Detachment of the labrum (Bankart lesion) can result in loss of the depth of the glenoid socket (arrow), which also leads to decreased stability of the joint
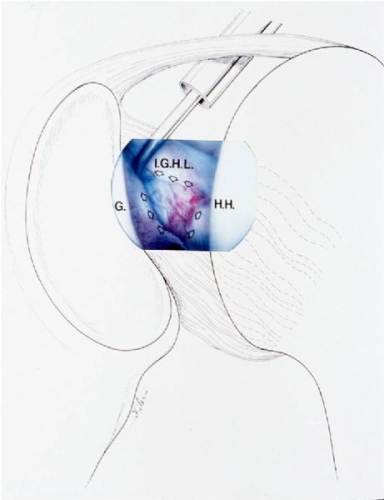
Fig. 15: In rare cases, a traumatic anterior instability can result in a capsular rupture (arrows outline injury).
In addition to ligament and labrum injury several other structures can be damaged when the shoulder dislocates.
NERVE INJURY: The brachial plexus are the complex of nerves that run in the front of the shoulder. When the humeral head (ball) dislocates out of the socket it can stretch or compress the nerves of the brachial plexus Fig. 16). This can result in weakness and loss of sensation (numbness) (Fig. 17). This can affect one or more nerves of the brachial plexus. The most commonly stretched nerve is the axillary nerve. This gives sensation along the side of the shoulder and it also carries the electrical impulses which cause the deltoid to contract and raise the arm overhead. Approximately 80% of the time such nerve injuries fully recover but this recovery may take many months.
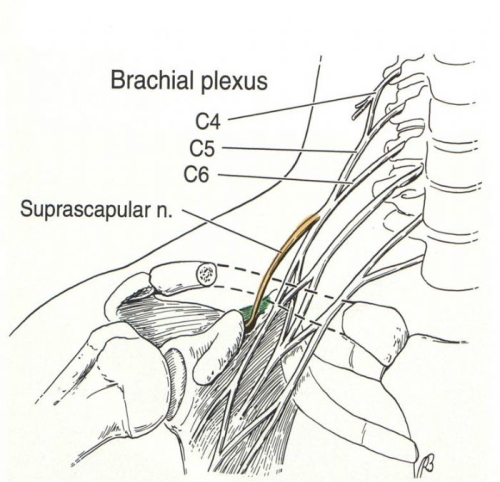
Fig. 16: The Brachial Plexus are nerves that come from the neck and run into the arm in front of the shoulder joint.
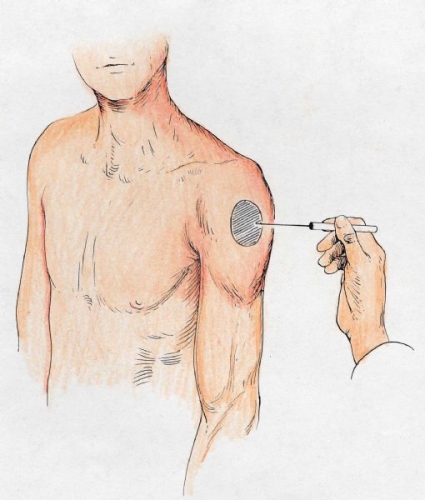
Fig. 17: The sensation on the side of the shoulder may be reduced if the axillary nerve is stretched
Rotator Cuff Tendon Injuries: Tears of the rotator cuff may occur in individuals over the age of 40 years when the individual suffers a traumatic injury; however, such tendon tears are rare in younger individuals. The reason for this is that with age the rotator cuff tendon weakens and may actually fail when it is stretched as the shoulder comes out of joint. It is very important for the physician to carefully evaluate the strength of the rotator cuff muscles (Fig. 18) after a dislocation and if there is any question of a tendon injury, an MRI should be obtained.
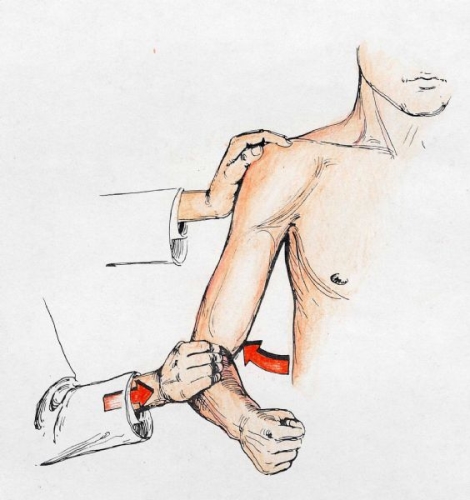
Fig. 18A: Abduction strength reflects the deltoid (axillary nerve) and the supraspinatus tendon of the rotator cuff.
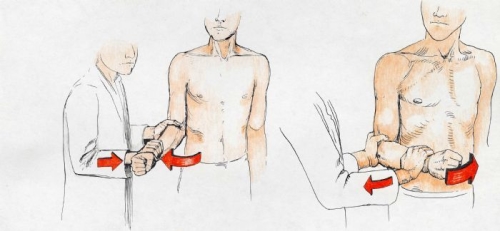
Fig. 18B: External rotation (out to the side) and internal rotation (inward) strength reflects strength of the infraspinatus and subscapularis muscles of the rotator cuff
Bony Injuries: In some cases of severe injury, the edge of the socket may fracture or the attachment of the rotator cuff (greater tuberosity) may pull off (Fig 19). In the case of multiple recurrences of shoulder dislocation, and especially if there have been one or more failed surgical stabilization procedures, there may be wearing down of the edge of the glenoid socket and development of a divot in the back of the humeral head (ball) (Fig. 20). The latter injury is called a Hill-Sachs lesion.
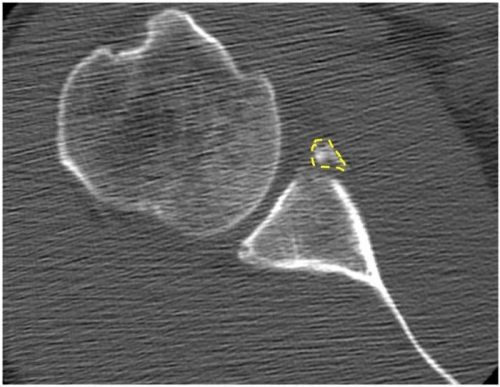
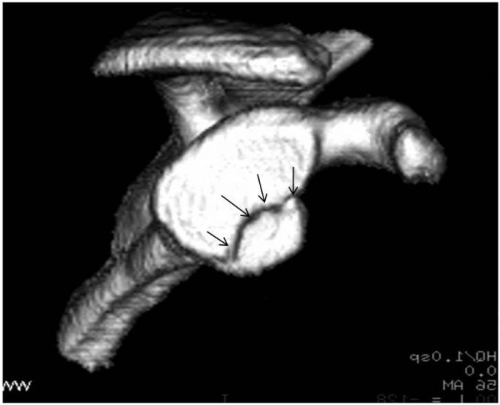
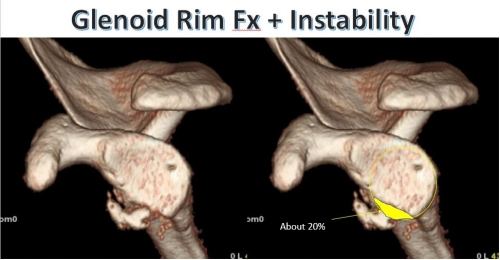
Fig. 19: Fracture of the edge of the glenoid socket (dotted line and arrows). These are CT scan studies.
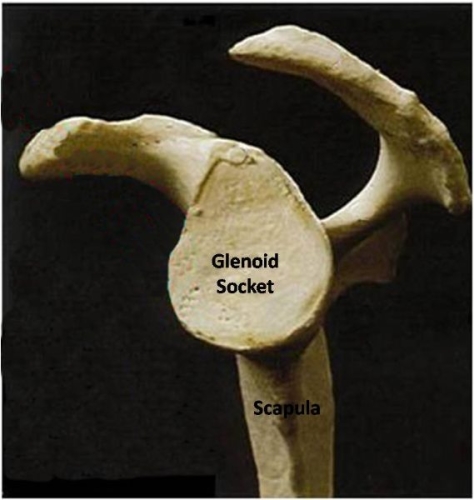
Fig. 20A: The normal glenoid socket is pear-shaped
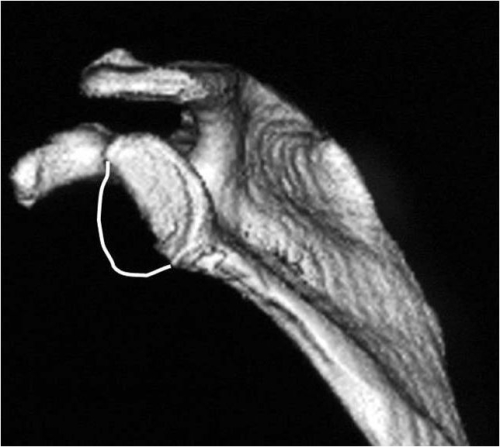
Fig. 20B: In the case of multiple dislocations, the socket can wear down up to half gone.
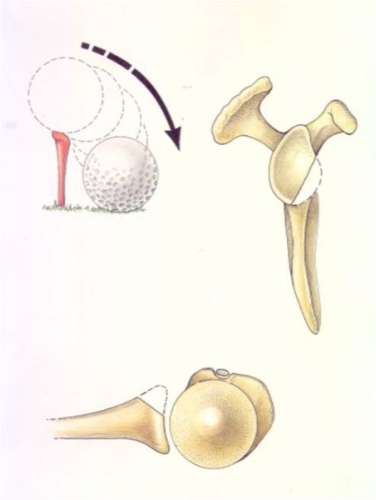
Fig. 20C: The instability that occurs is analogous to a golf ball falling off a fractured tee
Conservative Treatment with Physical Therapy:
If an acute dislocation occurs, the shoulder is immobilized in a sling for a period to allow the inflammation and pain to resolve. The length of time that the arm should be kept in a sling and the position of immobilization have been the subject of controversy. While some surgeons have suggested that 3 weeks of immobilization in a sling with the arm out to the side may reduce the likelihood of a recurrence of instability, recent studies have concluded this is not the case. Furthermore, the length of immobilization does not affect the risk for future shoulder instability. So our current treatment consists of immobilization for a week or two and then beginning a physical therapy program to recondition the muscles about the shoulder girdle. If the individual is an athlete, a program of therapy continues until strength is normal and there is no apprehension (pain and worry about dislocation) when the arm is brought out to the side. Return to sports is then possible; however, there is a significant risk of recurrent instability especially in young male athletes. Bracing can be used to increase a sense of security for the athlete, but there is no evidence this will prevent another episode of instability.
The likelihood of recurrence of instability is mostly associated with age, so an individual who is 40 years of age has less than a 50% chance of recurrence, while a 17 year old might have a risk greater than 90%.
Operative Stabilization of Shoulder Instability:
Surgical stabilization is indicated when instability recurs and becomes a chronic problem. The decision for surgical repair after an initial episode is influenced by a number of considerations. If there has been a fracture of the glenoid (socket) that remains displaced, surgery is indicated to restore stability and congruity to the joint. In the absence of a fracture, a consideration of the individual’s risks for instability and affect on athletic participation must be considered. If an athlete is young and if they will be involved in a collision or contact sport, they must be made aware that nonoperative treatment may place them at risk for a second dislocation and if this occurs during the athlete’s season it may end that season of competition. An alternative would be to have surgery in the off-season in order to ensure a lower risk of instability the following competitive season.
Arthroscopic vs Open repair of shoulder instability:
In the absence of a boney injury, the goal of surgery is to restore stability by repairing the Bankart lesion and any capsular stretch or rupture. In the majority of cases, this can be performed as an arthroscopic surgery. This surgery involves placement of anchors (plastic, metal, or absorbable) into the edge of the glenoid socket. Sutures from these anchors are then placed arthroscopically through the labrum and capsule. The sutures are then tied down, reattaching the labrum and capsule. This restores tension to the ligaments (hammock) and it restores the socket depth lost when a Bankart lesion occurs (Fig. 21).
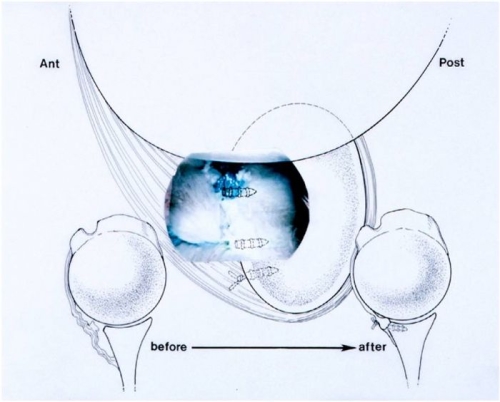
Fig. 21: Before and after an arthroscopic Bankart repair
Advantages of an Arthroscopic Repair vs an Open Repair: The current techniques and technology allow for results that are equivalent with both approaches; however, there are major advantages to the arthroscopic approach. These include less pain than with an open approach and the possibility to have the surgery under a local anesthesia as an outpatient (going home after surgery). With an arthroscopic approach, there is no need to disrupt normal tissues like the rotator cuff, which may be required with an open approach. Furthermore, the risk of infection is theoretically lower with an arthroscopic approach than with an open approach.
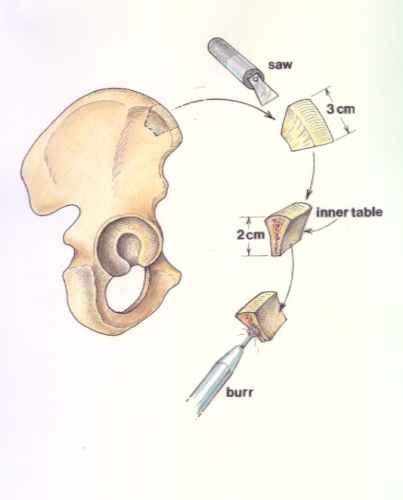
When is an Open approach required?: In over 90% of cases, an arthroscopic approach is feasible. In the remaining 10%, an open approach may be required to deal with bone loss (as described above) or with a capsular injury (very rare). In the case of loss of bone along the anterior (front) of the glenoid socket, a soft-tissue Bankart repair has a high likelihood of failure. Instead, a bony procedure must be performed. Our approach is to perform an operation called a Latarjet Procedure. This technique was named for the French Orthopaedic Surgeon who described it. It involves transfer of a bone (coracoid process) in the front of the shoulder into the front part of the scapula so that it acts to restore the glenoid socket surface. Attached to this bone is a tendon (conjoined tendon) that acts as a sling in the front of the shoulder, thus restoring the hammock effect described above (Fig. 22)
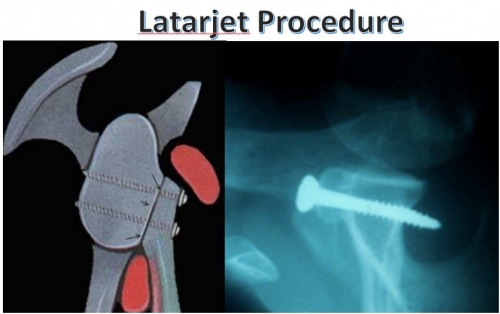
Fig. 22A: Latarjet Procedure (Image courtesy of Dr. Gilles Walch). The transferred coracoid process is fixed in place with bone screws and restores the glenoid socket shape
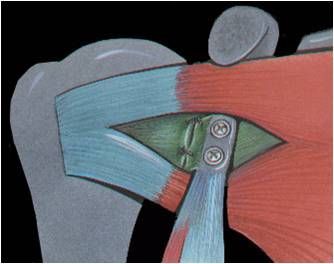
Fig. 22B: Latarjet Procedure (Image courtesy of Dr. Gilles Walch). The tendon is transferred through a split in the subscapularis muscle, so no muscles are detached and repaired with this procedure
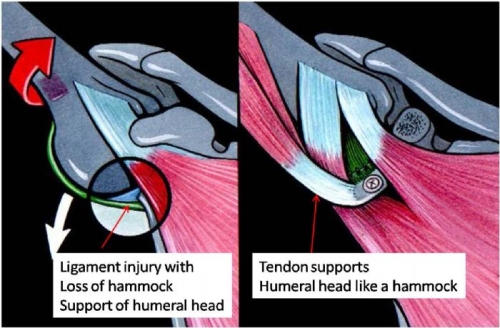
Fig. 22C: Latarjet Procedure (Images courtesy of Dr. Gilles Walch). When the arm is raised overhead and rotated externally (outward) as in a throwing motion, the conjoined tendon attached to the bone acts as a sling supporting the humerus in the joint like a hammock