Our Value Commitment

The Boston Shoulder Institute is committed to delivering “Value-Based” Shoulder Care. This means our primary purpose is to always put the patient first. We aim to achieve this goal through the following processes:
1. Communication: The first step in providing value is to listen clearly to the patient and understand not only the problem but also the impact of the problem on the patient’s life and overall well-being. Once we have formulated an opinion about the possible causes of the patient’s problem, our goal is to clearly communicate the nature of the problem. It is essential to have patients understand the problem so they can be smarter consumers of their care. In most cases, the patient will need to make decisions about their treatment and having a better understanding of the risks and benefits is essential to such decision-making. This is called shared decision-making. We achieve this through direct discussion with the patient and use of our website as a teaching aid.
2. Accessibility: Value is also delivered by a process whereby we make ourselves accessible to our patients. This is achieved through either timely email communication, telephone communication or written communication (All communication is in compliance with HIPPA laws). There are many who assist us in this process. This includes our office managers, physician assistants, nurse practitioners, nurses, and other doctors.
3. Accountability: We believe in being accountable for the value of care we deliver. This includes not only delivering reliable outcomes with low risk, but also thoughtful use of resources, such as x-rays, MRI’s and other testing. We also believe in active management of physical therapy in order to deliver the best value to our patients. As such we require that therapists caring for our patients to adhere to our proven protocols of care and communicate updates of each patient’s progress throughout their recovery.
4. Transparency: True value must be delivered with transparency. This means our processes and outcomes must be reported openly. E.A. Codman, the father of shoulder surgery in the United States, worked in Boston in the early 19th century and proposed the “End Result” concept. This meant the patient’s outcome was the only important measure, and he believed in “End Result Report Cards” so patient would know the value of the care they were to receive. Our pledge to our patients is to be transparent about our results in specific conditions we treat. These include the entire spectrum of shoulder problems such as rotator cuff tears, shoulder instability, arthritis, and fractures. Our “Quality Measures” section on our website (http://www.bosshin.com/quality_measures) presents our ongoing reporting of our patient satisfaction rates and our complication rates for all the surgical procedures we perform.
5. Care Coordination: Healthcare delivery is very complicated and often confusing for patients. Even though shoulder care would seem to be a simple problem compared with heart disease and cancer, patients often have very relevant health issues which impact the care of their shoulder problems, so communication and coordination of care with other healthcare providers is an essential part of delivering value. We recognize the importance of methodical and thoughtful communication in order to minimize risk of surgery and optimize our patient’s care. This may be as complicated as communicating with a patient’s cardiologist or neurologist or as straightforward as coordinating physical therapy to ensure accountability and effectiveness of a patient’s recovery after surgery.
6. Critical Introspection: Perhaps the most important initiative we are taking to improve value is our relentless pursuit of the most reliable treatment for specific conditions. All of our care is delivered based on three key principles:
a. First, what does the current literature show is the best treatment for a given condition?
b. Second, what does the most current research show is the best science in support of a given treatment for a patient’s condition?
c. And third, what would we choose for ourselves or one of our family members if we were to select the best treatment? Our patients deserve no less.
7. In order to achieve optimum results we are constantly evaluating our outcomes and looking for the best practices to ensure low risk and high rate of success. We systematically review our outcomes prospectively and retrospectively. Our work is presented transparently for our patients in the “Quality Measures” portion of our website (http://www.bosshin.com/quality_measures) as well as in the “Modules” section of our website (http://www.bosshin.com/shoulder_modules/).
We also believe that patients should know that surgeon experience (volume) has a direct correlation to their potential outcome. Indeed, our experience as specialists in care of shoulder problems adds to the value we deliver to our patients. The literature is very clear on this (Click Link Below)
(http://bosshin.com/_userfiles/Black,%20Eric%202013%20JSES-%20Value%20Based%20Shoulder%20Surgery-%20Practicing%20Outcomes%20Driven,%20Cost-%20Conscious%20Care.pdf)
In conclusion, it is our privilege to care for individuals with shoulder problems and we have committed ourselves and our careers to providing the best possible value in shoulder care. Moreover, we believe our active collaboration with our colleagues and with other stakeholders (insurers, worker compensation providers, our hospitals, vendors) distinguishes the value we provide from other caregivers in the region.
Value-Based Shoulder Care: Our Pledge to Our Patients
“Value” means different things to different people. As defined by many healthcare experts, value is the “OUTCOME” divided by the “COST OF OVERALL CARE” (see figure below). However, we believe the patient is the most important individual in defining the “value” of care. For the patient, value of an intervention should mean several things. First, it should mean restoration of function and elimination of pain. Second, it should mean lack of complications of treatment. While surgical intervention to solve a shoulder problem always entails some level of risk, minimization of this risk is inherent to delivering value.
“Value” should also include a process of informing patients in order to make them better consumers so they can make smart decisions about their care. Most patients only know they have pain and limited function, but not the adequate information to make an educated choice regarding their care. A patient’s path to recovery usually includes different treatment options, each with their own inherent level of risk. The “value” initially delivered by the physician is to clearly and coherently inform the patient what their problem is and help them navigate through their available options. This is called “shared decision-making”.
Other more indirect measures of value relate to the patient’s experience. These include ease of accessing the expert care they deserve as well as the experience itself (which can be very confusing and complicated). Time spent in the physician’s office is often frustrating, but may be less so if the patient leaves with a clear understanding of the plan for their care. Open lines of communication are essential to provide value to the patient during the process of care. This is best facilitated by direct communication with the physician or his or her care extenders (which may include physician assistants, nurse practitioners, or other physicians).
How about other Stakeholders in the Value of care delivery? The figure below shows that many different groups interact in the delivery of value:
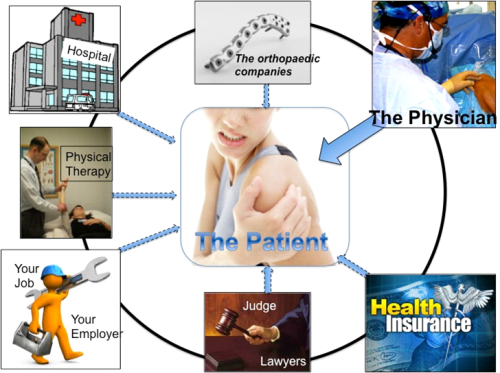
The “Third Party Payor” is the insurance company, which pays most of the bill for the patient’s care. Understandably, this stakeholder is interested in the overall cost of care. For the insurer, this includes use of resources (surgery, physical therapy, imaging like MRI’s). In the value equation (see below), cost represents the denominator of the equation. Unfortunately, for many insurance companies, the priority is on cost reduction rather than influencing overall value by improving the outcome.
Actually, all stakeholders in delivering value have a conflict of interest. The “third party payor” (insurer) has a goal to control and reduce costs and this may adversely affect the overall value in some circumstances.

The “Physician” (Orthopaedic Surgeon) is the principle stakeholder, other than the patient, most concerned about the outcome and the overall value of the care. To be fair, income may also play a role and this can be a positive or a negative motivator. While the orthopaedic surgeon is motivated to provide the best outcome, his (her) conflict is the potential income derived by surgical care provided. Ideally, it should be about “value” not about “volume” and a patient-first approach means careful consideration for non-operative as well as operative options. The orthopaedic surgeon makes the diagnosis and orders the testing required for both diagnosis and treatment. The overall cost (denominator) is affected by the surgeon’s decisions. Thus, the orthopaedic surgeon is the stakeholder who influences both the numerator and denominator more than any other stakeholder.
The “Hospital” is the healthcare facility where you receive your care that may be an outpatient surgical center. The hospital is, of course, interested in the “quality” of your care and the ultimate “outcome”. However, it must also manage its costs and create a margin or profit in order to remain financially healthy and continue to be a resource for future patients. Therefore, care delivery without complication and at fair cost is the principle aim of the hospital. Nevertheless, resources are often poorly managed and the more resources that are used (i.e. MRI scans, physical therapy, surgical implants), the more the hospital charges. In fact, hospital charges are currently the single biggest cause of overall cost of care, and the more care that is delivered, the greater the charges that are created. This represents a potential conflict in the hospital’s mission to deliver value. Thus, cutting costs is not the main focus of the hospital. In contrast, the fee paid for the surgeon’s care constitutes only 5-7% of the overall cost of a patient’s care, if the patient has surgery.
The “Orthopaedic company” means all vendors who provide devices and implants for the patient’s care. For example, if a patient has arthritis, a joint replacement may be required. If the patient has a fracture, a plate and screws might be required. In most cases, patients require a sling or shoulder immobilizer after surgery. All of these devices add cost to care. In fact, the single biggest charge for a patient undergoing a joint replacement is the cost of the implant. “Orthopaedic Companies” have a mission to provide quality products and also deliver a profit. Indeed, it is their fiduciary responsibility to deliver value to shareholders of their company, so profit is their biggest motive. This is the inherent conflict of interest in the value delivered by the orthopaedic company. This may not always be a negative, as it can create competition for implants and devices, which can drive down cost overall while still maintaining high quality.
“Physical Therapy” is an important part of recovery from any shoulder injury. However, there is a huge variability in the quality of the therapy delivered and the quantity utilized. This important resource contributes to both outcome and cost and must be managed thoughtfully by the orthopaedic surgeon in order to ensure value for the patient. Unfortunately, sometimes too much physical therapy is delivered and quality is not measured.
“The Job and the employer” are important indirect measures of value of a patient’s care. This is especially the case in “work-related injuries” where the goal is to return the injured worker back to his or her prior employment. Sometimes however, the employer may have an unrealistic expectation for the patient’s recovery, and put these goals ahead of the patient’s best interest. This is also a potential conflict of interest in delivering value to the patient. Thoughtful management of the process and resources by the orthopaedic surgeon is the best way to deliver value to both the patient and the employer.
“Lawyers and Judges” unfortunately have become an important part of the Value equation in some cases. This is especially the case in liability suits after an injury or in work-related injuries. Such legal implications certainly can pose a potential conflict of interest in delivering value to the patient. Value can be delivered to these stakeholders through clear communication, transparency and realistic expectation for recovery. Such management by the orthopaedic surgeon may help remove the legal and financial barriers to appropriate care for the patient.
