Sternoclavicular Joint
William Bragg, MD, MBA, Alex Girden, BA, Jon JP Warner, MD (November 4, 2013)
The sternoclavicular joint is located towards the center of your chest and is the point at which the clavicle (collarbone) and sternum (breastbone) meet (Figures 1 and 2). It is an important joint because it is the only joint connecting the upper limb to the rest of the body.
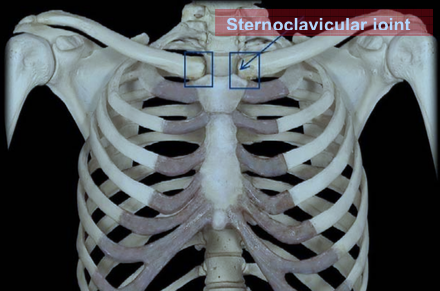
Figure 1: The sternoclavicular joint: bony anatomy Source: www.studyblue.com
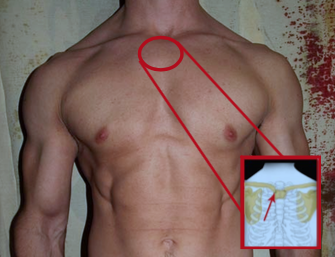
Figure 2: The sternoclavicular joint: exterior appearance
Source: http://www.dme-direct.com/shop-by-injury/back-injuries/sternoclavicular-joint-separation
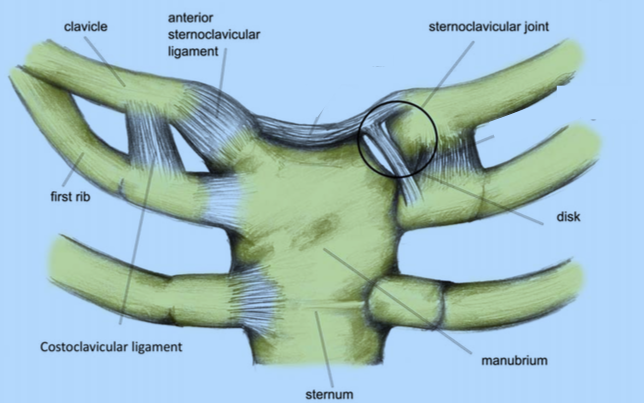
Figure 3: Bones and ligaments of the sternoclavicular joint
Source: http://www.sportsinjuryclinic.net/sport-injuries/shoulder-pain/sternoclavicular-injury
Although the sternoclavicular joint is important in providing stability to the upper limb, little stability is actually provided by the bony joint surface itself. The area of contact between the clavicle and the sternum is relatively shallow. As a result the main source of stability of the sternoclavicular joint comes from the surrounding ligaments instead of the connection between the bones (Figure 3). The primary ligament that provides this stability is the capsular ligament that is divided into the anterior (front) and posterior (back) sternoclavicular ligaments. The posterior sternoclavicular ligament is the more important of the two as injury to it may result in both anterior and posterior instability at the joint. The anterior segment acts as a secondary stabilizer to limit motion at the joint. There is also a ligament in the joint space itself that provides cushioning and prevents the clavicle from shifting towards the middle of the chest. The costoclavicular ligament limits superior and inferior rotation. Surrounding muscle and other minor ligaments provide additional stability around the sternoclavicular joint (Figure 4).
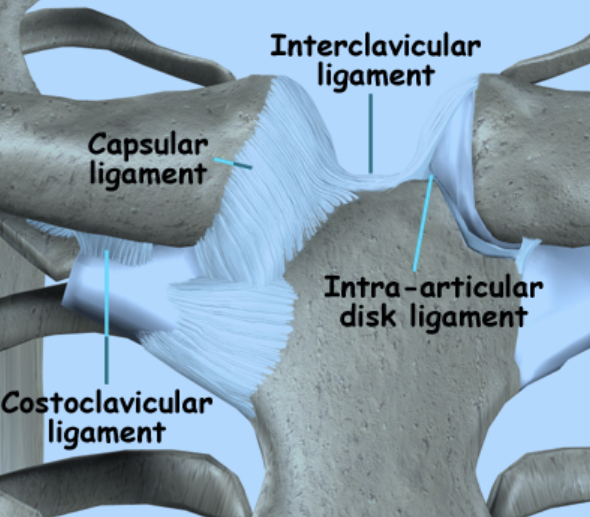
Figure 4: Ligaments of the sternoclavicular joint
Source: http://www.eorthopod.com/content/sternoclavicular-joint-problems
The sternoclavicular joint is very close to several very important anatomic structures. Just behind this joint in the chest are several important blood vessels as well as the swallowing and breathing tubes (the common carotid artery, subclavian vessels, lungs, esophagus, and trachea). These structures can be at risk for injury with a surgery performed in this area (Figure 5).
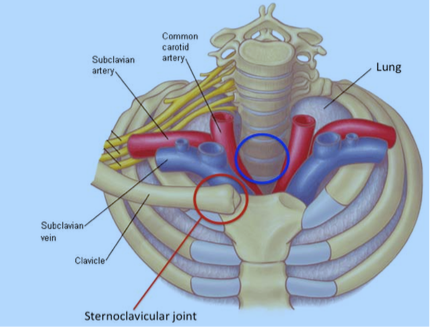
Figure 5: The sternoclavicular joint and nearby structures. Red circle: Sternoclavicular joint. Blue circle: The esophagus and trachea (not pictured) sit in this area behind the sternoclavicular joint. The structures are at risk during surgery.
Source: https://online.epocrates.com/data_dx/reg/592/img/592-5-iline.gif
The soft-tissue pad of cushioning at the sternoclavicular joint (between the collarbone and breastbone) is called the intra-articular disc and can be a source of pain (Figures 6 and 7). The disc can develop a tear, either as result of injury, or just from wear and tear, which can be very painful. Someone with this injury may feel pain and stiffness at the joint but may also have clicking and popping from the torn disc. Although this injury can very often be managed non-operatively, in cases of unrelenting pain, the disc can be removed through surgery, eliminating the source of the pain.
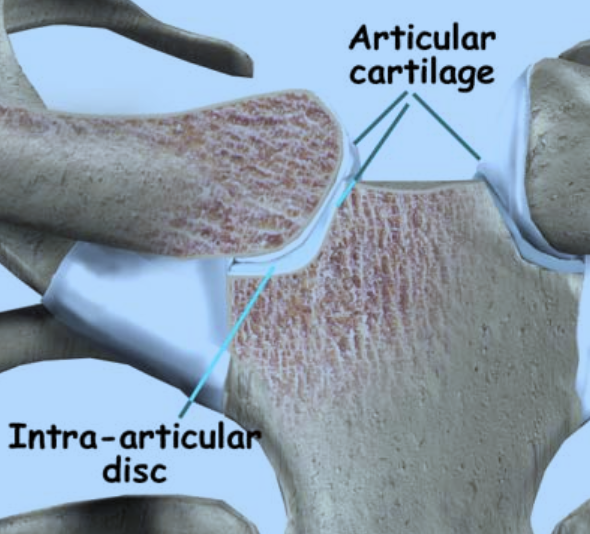
Figure 6: Intra-articular disc of the sternoclavicular joint
Source: http://www.fernleyphysicaltherapy.com/Injuries-Conditions/Shoulder/Shoulder-Issues/Sternoclavicular-Joint- Problems/a~372/article.html
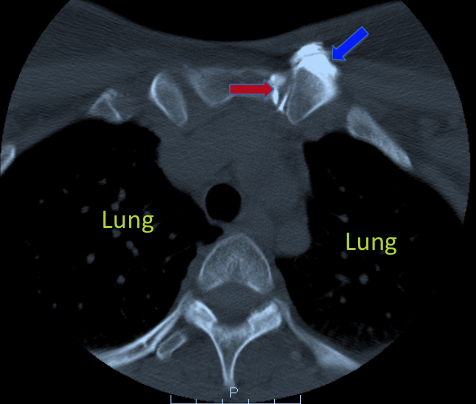
Figure 7: Computed topography arthrogram of the sternoclavicular joint: This CT scan shows the sternoclavicular joint (red arrow) after it is injected with a dye. As the disc is torn, the dye outlines the entire disc and escapes outside of the joint (blue arrow). This is a sign of injury at the disc.
Source: Image courtesy of Dr. Jon JP Warner
With advancing age, arthritis can develop in the sternoclavicular joint, much as it can in larger joints such as the hip and knee. Although this is an uncommon finding it may manifest as both swelling and pain. Both sides may be affected but it is not unusual to find one side is more symptomatic than the other. While this is a degenerative process with loss of cartilage, bone spur formation, and narrowing of the joint space, it is usually associated with some trauma (Figure 8 and Figure 9).
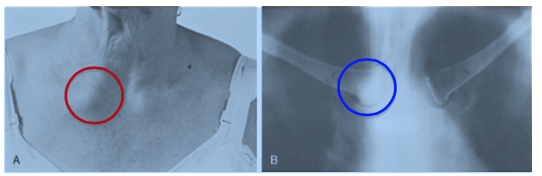
Figure 8: Sternoclavicular arthritis in a 67-year old female. Picture A shows prominence of the right sternoclavicular joint due to swelling from arthritis (red circle). Picture B is an x-ray showing narrowing and degeneration of the joint space from arthritis (blue circle).
Source: Rockwood CA, Green DP [eds]: Fractures [3 vols], 2nd ed. Philadelphia: JB Lippincott, 1984
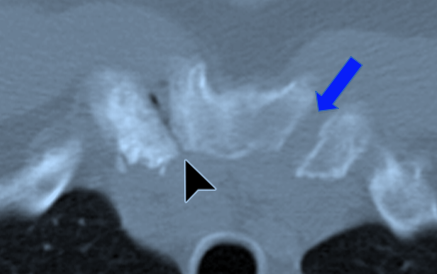
Figure 9: Arthritis of the sternoclavicular joint: The right sternoclavicular joint in this patient is narrowed, with loss of cartilage at the joint space (black arrow). This is a characteristic sign of arthritis at this joint. The blue arrow is at the left sternoclavicular joint, which is normal. Notice how much wider the normal joint is.
Source: http://radiographics.rsna.org/content/29/3/839/F16.expansion
Although infection in the sternoclavicular joint (septic arthritis) is relatively rare, it can also be a source of pain and swelling with associated fevers and chills. Untreated infection can potentially progress to systemic and life-threatening illness. Septic arthritis of the sternoclavicular joint is most commonly associated with HIV infection, alcoholism and IV drug abuse, infected central catheters, and renal dialysis.
Loss of blood supply to the end of the clavicle (osteonecrosis) (Friedrich’s disease of the sternoclavicular joint) is a rare cause of pain at the joint, This process occurs in the absence of any significant trauma or infection and is usually a self-limited process which is well managed with anti-inflammatory medication and restriction of activity.
A severe trauma can result in disruption of the ligaments around the joint causing the medial clavicle to dislocate (Figure 10). A direct blow to the medial clavicle can occur if the individual falls on the shoulder, which may result in a posterior dislocation of the end of the clavicle (Figures 11, 12, and 13). Such displacement pushes the clavicle towards the important structures behind the sternum (breast bone) (Figures 13, 14, and 15). Therefore a posterior dislocation can cause the patient to cough or become hoarse with difficulty breathing, and can even produce a sense of choking if the trachea (breathing tube) is compressed (Figure 14). Circulation to the arm on the same side can be decreased from pressure on blood vessels behind the clavicle. A posterior dislocation can potentially be an emergency as the dislocated clavicle end can cause a collapsed lung or direct injury to one of the major blood vessels. With a posterior dislocation the usually easily palpable end of the clavicle will appear less prominent.
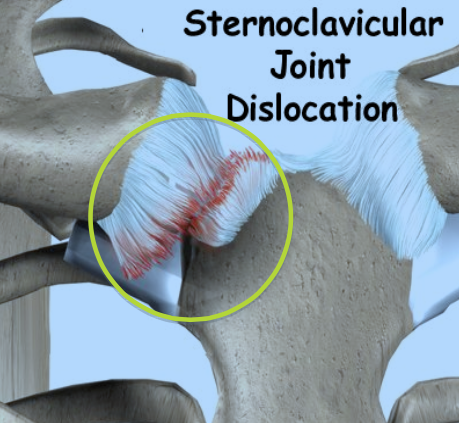
Figure 10: Sternoclavicular dislocation. When the joint is dislocated, the ligaments that hold it in place are torn, as depicted here.
Source: http://www.lakeviewphysio.ca/media/img/1013/shoulder_stclav_intro01.jpg
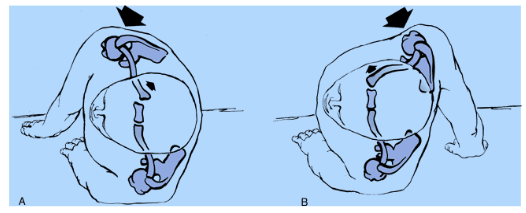
Figure 11: Sternoclavicular dislocation. In Picture A, a blow to the back of the shoulder causes a posterior sternoclavicular dislocation. In Figure B, a blow to the front of the shoulder causes a posterior dislocation.
Source: Rockwood CA, Green DP [eds]: Fractures [3 vols], 2nd ed. Philadelphia: JB Lippincott, 1984
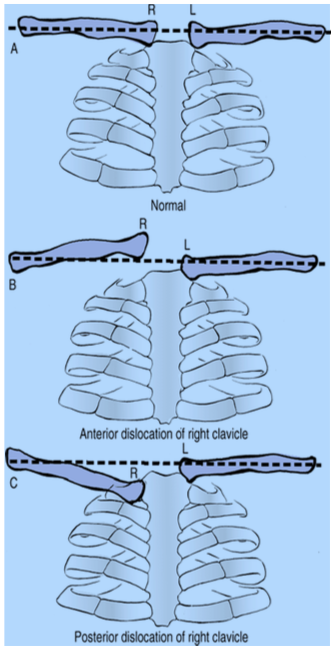
Figure 12: Sternoclavicular dislocation: Picture A shows the normal relationship of the clavicles (collar bones) to the breastbone. In a right anterior dislocation (Picture B), the right clavicle becomes elevated and prominent. In a right posterior dislocation (Picture B), the clavicle becomes lowered and depressed.
Source: http://www.msdlatinamerica.com/ebooks/RockwoodGreensFracturesinAdults/sid980598.html

Figure 13: Sternoclavicular dislocation. This view, looking down on the body from above, shows how the clavicle shifts towards the back of the body with a posterior dislocation.
Source: http://www.eorthopod.com/images/ContentImages/shoulder/shoulder_sternoclavicular/shoulder_stclav_cause01.jpg
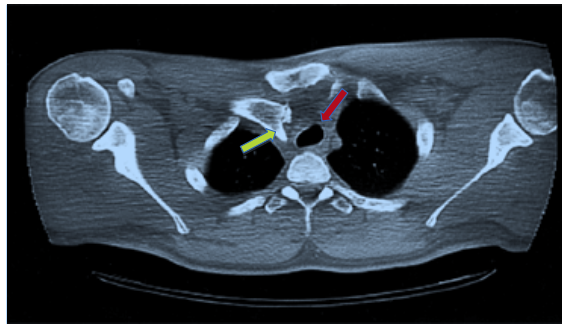
Figure 14: Computed tomography (CT scan) of a posterior sternoclavicular dislocation. Note the clavicle is pushed deeper into the chest (yellow arrow), placing the trachea (breathing tube) in danger (red arrow: trachea). The trachea is pushed deeper into the chest, away from its usual spot; this may cause breathing difficulty and can be life-threatening
Source: Rockwood CA, Green DP [eds]: Fractures [3 vols], 2nd ed. Philadelphia: JB Lippincott, 1984
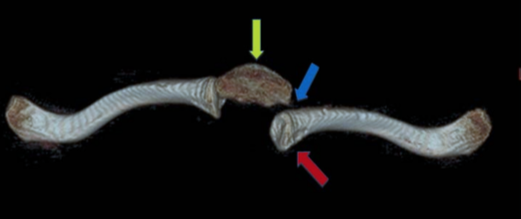
Figure 15: 3D CT scan of a posterior sternoclavicular dislocation. The clavicle (red arrow) is pushed deeper into the chest behind the breastbone (yellow arrow) in a posterior dislocation. There is now a gap (blue arrow) between the breastbone and the clavicle.
Source: Image courtesy of Dr. Jon JP Warner
Anterior dislocation, which is the most common type of SC joint instability, typically results from indirect trauma, such as a lateral blow to the arm that pushes the midline clavicle forward or from rolling/compression motions that force the clavicle to dislocate to the front of the sternum (Figures 10, 11, 12, 16, and 17). The medial end of the clavicle may be visible above the sternum.

Figure 16: Anterior sternoclavicular dislocation. The arrow highlights the prominence of the joint after it moves forward after dislocation.
Source: http://accessemergencymedicine.com/loadBinary.aspx?fileName=simo6_c016f039t.jpg

Figure 17: Anterior sternoclavicular dislocation.
This view, looking down on the body from above, shows how the clavicle shifts towards the front of the body with an anterior dislocation.
Source: http://www.eorthopod.com/images/ContentImages/shoulder/shoulder_sternoclavicular/shoulder_stclav_cause01.jpg
For traumatic injuries that result in anterior sternoclavicular sprain or subluxation (incomplete dislocation), non-operative treatment with rest, ice, and analgesic medication (e.g. narcotics or anti-inflammatory medication) typically is sufficient. For persistent, recurrent subluxation, reduction can be achieved by directing the shoulders posteriorly and towards the midline. A sling / figure-of-eight dressing may be used in the early period for comfort and stability for up to 6 weeks.
If the sternoclavicular joint dislocates anteriorly, nonsurgical management is usually the first option but there may be residual cosmetic deformity and instability at the joint (Figure 16). Closed reduction is the preferred method of intervention; this involves giving the patient medication to relax and sedate him or her so that the joint can be put back into place. Sometimes, the patient may need to be placed under general anesthesia in the operating room (this is more typical for reduction of posterior dislocations). The patient lies on his or her back and a pad is placed between the shoulder blades. Posteriorly directed force is then applied directly to the protruding medial clavicle. This maneuver causes the sternoclavicular joint to reduce. The patient is then placed into a sling or figure-of-eight dressing for 6 weeks to allow for healing. Although a formal surgical incision can be made to look directly at the joint, this carries significant risks due to the delicate structures around the joint (major blood vessels, the airway) and is typically not pursued. Usually, patients do not have significant disability related to residual prominence of the clavicle or instability. As a result, surgery is rarely pursued and many individuals maintain near normal range of motion and can continue to perform manual labor or athletic activities.
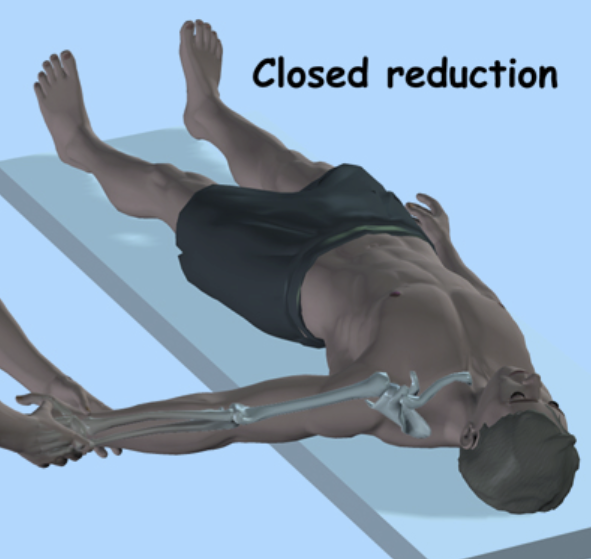
Figure 18: Closed reduction of a posterior sternoclavicular dislocation.
Source: http://www.orthogate.org/patient-education/shoulder/sternoclavicular-joint-problems.html
Posterior dislocations are more difficult to treat as the displaced end of the clavicle is behind the sternum and very close to structures, that when injured, can lead to life threatening complications. Reduction of posterior dislocations by orthopaedic surgeons should also be performed in the operating room with general anesthesia. A cardiac or thoracic surgeon should be available to assist if there is concern for penetration into or around any of the great vessels behind the joint.
The patient is again placed on his or her back with a bump between the shoulder blades (Figure 18). The arm is extended over the edge of the table and a combination of traction, arm extension, and posterior force on the shoulder is used to reduce the joint. Sometimes a towel clip may be necessary to grasp the end of the clavicle after a surgical incision is made to pull it forward.
When this closed technique fails, an open surgical procedure with a larger incision is necessary (with a thoracic surgeon immediately available). A larger incision is made over the joint in order to fully expose the ends of the clavicle and sternum. Often, once the clavicle is back in place, the joint may be stable. If this is not the case and there is persistent instability, a surgical reconstruction of the sternoclavicular ligaments may be performed.
Use of such grafts is necessary when the ligaments are torn beyond the point of repair (Figure 19).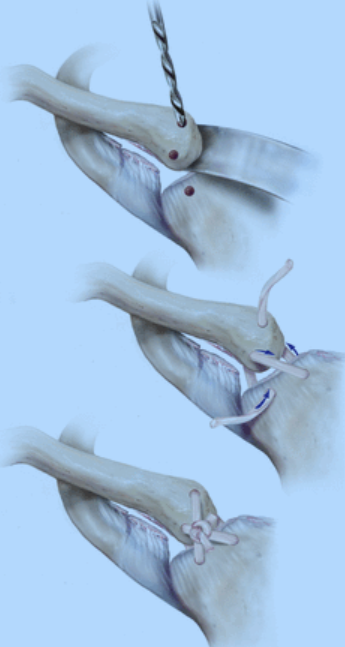
Figure 19: Sternoclavicular joint reconstruction with allograft (cadaver tendon). Drill holes are made into the bone and the tendon is threaded through and tightened down to restore stability. A small part of the collarbone right next to the breastbone may also be removed.
Source: The American Journal of Sports Medicine, http://ajs.sagepub.com.laneproxy.stanford.edu/content/early/2013/08/16/0363546513498990/F2.expansion.html
Following surgery, patients wear a sling or figure-of-eight strap for 6 weeks at all times. Range of motion of the elbow, wrist, and hand is maintained for light activity. Immediately following surgery, pendulums may be performed at the shoulder but dedicated physical therapy does not start until at least post-operative week four. At that time gradual progression of passive then active range of motion is initiated. Strengthening is deferred until full range of motion is obtained at 9-12 weeks.
Sternoclavicular dislocations account for less than 3% of all traumatic joint injuries. As this is a relatively rare injury, there are few large studies on the long-term results following treatment of this injury.
A 2011 study by Grohl2 involved 21 patients with sternoclavicular joint dislocations. Of the 21 patients, only 8 were successfully treated with closed reduction (i.e. no surgery). The remaining 13 required surgery. At 5-year follow-up, 18 of the 21 patients had good or excellent results in the ratings for pain, strength, motion, sports, and daily activities. Some patients still had some pain and difficulty with certain activities but overall these patients did very well after surgery.
Another study by Guanin 2013 looked at surgery in 6 patients with anterior dislocations3. They found that all 6 patients had good shoulder motion and no instability after treatment. Five patients had no pain and only one patient had mild pain. These patients did well in follow-up up to four years later, although one patient did develop arthritis and need more surgery.
Another study looked at treatment for either anterior or posterior sternoclavicular dislocation in 251 patients1. 80% of patients had good/excellent results with either a closed reduction or with surgery. However, patients with anterior dislocations tended to do better without surgery.. Patients with posterior dislocations did well regardless of whether they had just a closed reduction or surgery.
