Reverse Shoulder Replacement
(Eric M Black, MD; Paul Yannopoulos, BA; Jon JP Warner, MD) May 2013
In a normal, or “anatomic” total shoulder arthroplasty, the ball and socket of the shoulder is replaced to mimic the shoulder’s natural joint anatomy and mechanics. The humeral head or “ball” is replaced with a metal implant made of cobalt chrome and titanium which resembles the head’s native size and anatomy. The glenoid, or “socket” is replaced with polyethylene (plastic) that is similar in size and shape to the natural glenoid anatomy. This procedure is typically indicated for patients with arthritis of the shoulder that have intact, or normal, rotator cuff tendons.
Figure 1: The anatomic total shoulder replacement, showing a polyethylene glenoid component and a cobalt chrome humeral head component.
A reverse prosthesis (also known as reverse total shoulder arthroplasty, or reverse shoulder replacement) is a newer technology that utilizes a “non-anatomic” shoulder replacement in patients who have shoulder arthritis and are without normal rotator cuff muscles and tendons. This prosthesis can also be used as a salvage procedure for failed surgery (i.e. for revising a failed total shoulder replacement) or in older patients with severe fractures of the proximal humerus (shoulder) that may be beyond surgical repair (due to loss of bone or a large number of fracture pieces).
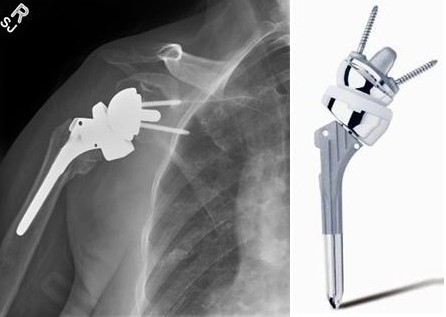


(Figure 2: Different devices are available and are chosen based on surgeon’s preference. As seen above, the ball and the socket are reversed. The polyethylene glenoid component is attached to the humeral stem, while the humeral head is fixed in the scapula)
The reverse shoulder prosthesis was originally developed in the 1980s in France by Dr. Paul Grammont (http://www.ncbi.nlm.nih.gov/pubmed/21210311), While this device enjoyed great success in Europe over the next several decades it was not approved by the FDA for use in the United States iuntil 2004.In the normal shoulder, the muscles of the rotator cuff help center the humeral head (ball) within the glenoid (socket) by providing a centralizing force to the joint. This helps counteract the upward force of the deltoid on the shoulder joint.
The rotator cuff muscles and tendons support elevation and rotation of the shoulder. (FIGURE 3) In patients without normal rotator cuff muscles such as with a rotator cuff tear or fracture, the deltoid muscle pulls the humeral head upward out of the joint so elevation of the arm is impossible. This can lead to arthritis which has been termed “rotator cuff tear arthropathy”. (Figure 4)
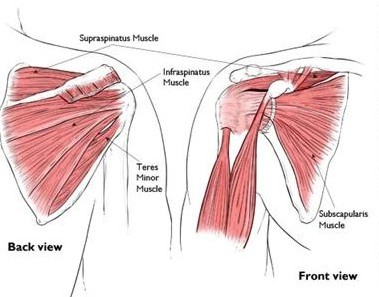
Figure 3: Showing the normal anatomy of the rotator cuff: Subscapularis (seen from the front), Supraspinatus, Infraspinatus and Teres Minor. These muscles and their tendons keep the humeral head centered on the glenoid through compression of the joint.
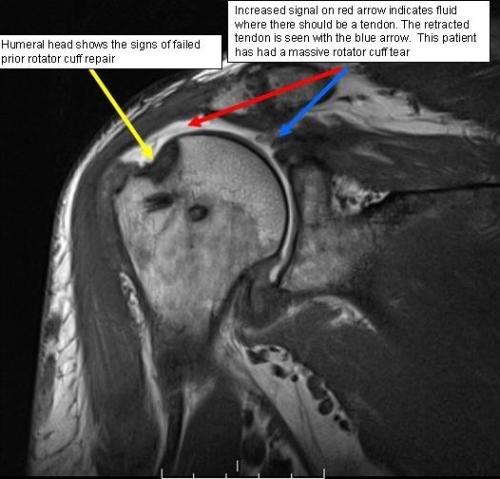
Figure 4: With a torn rotator cuff tendon, seen in the MRI image, a patient may have difficulty lifting his or her arm. The torn tendon may cause inflammation and irritation that make movements painful. In the MRI, one can visualize the fluid where there once was tendon. The tendon has fully torn and retracted to the blue arrow.

Figure 5: The humeral head shifts upward, due to the loss of compression from the rotator cuff. The XRay reveals the superior migration of the humeral head in the right image- the ball is no longer ‘in line’ with the socket as seen in the left image.
In a reverse shoulder arthroplasty, or reverse prosthesis, the ball of the shoulder (humeral head) is replaced with a socket, and the socket of the shoulder (glenoid) is replaced with a ball. This allows for a fixed fulcrum so the deltoid muscle can now elevate the arm without a normal rotator cuff. The prosthesis is secured in place using screws in the ball portion and either cement or bone growth onto the prosthesis for the socket/stem portion.

Figure 5: When the humeral head moves upward out of the socket, the fulcrum for rotation is lost (seen on the left). A reverse prosthesis brings the point of rotation lower and restores a fulcrum of rotation. The socket can now rotate around the ball, allowing for the ‘lever’ of the deltoid to raise the arm.
In some patients, the rotator cuff tendons are irreparable due to poor quality or actual absence. This may be the case in a chronic rotator cuff tear, failed prior surgery, or after a fracture. Sometimes rotator cuff tendons can fail after a shoulder replacement. (see figure 6)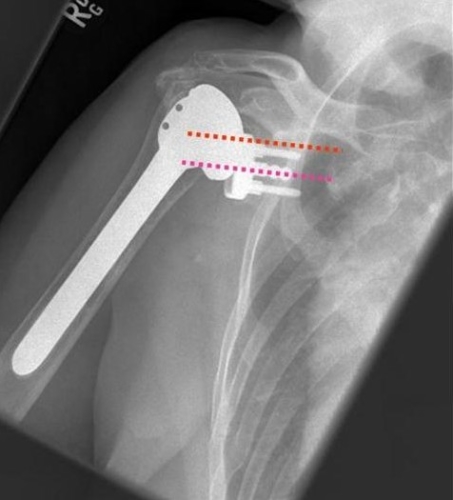
Figure 6: The picture demonstrates that the prosthesis (humeral component) has shifted upward due to rotator cuff insufficiency. The purple dotted line shows where the center of the humeral head should articulate, while the red dotted line shows the actual location- too high.
Reverse Total Shoulder Replacement: Our Experience
Preoperative preparation:After the decision for surgery is made, you will likely be asked to obtain clearance for surgery from your primary care doctor and/or cardiologist (if you have one). More than likely, you will undergo a more advanced imaging study such as a CT or MRI prior to surgery, if you have not had one already. It is important to talk to your surgeon if you are having new symptoms such as skin infections, shortness of breath, chest pain, or any other concerning symptoms.
Your Surgery and Hospital Stay:
Surgery will take place at one of our main hospitals (MGH or BWH). Depending on the preference of your surgeon, you may receive a preoperative nerve block for additional pain control (ISB – Quality Measures). Surgery will take place under general anesthesia, and usually lasts about 2 hours. If your case has a higher complexity, it may take longer. This is especially the case if surgery is being done to revise a failed prior shoulder replacement. The total time in the operating room may also be longer due to anesthesia requirements and setup time.
You are then admitted to the hospital for about 2-3 days, and are discharged either home or to an extended care facility depending on your level of need and independence. This is typically determined in collaboration with a case manager, physical/occupational therapist, and your surgeon. While you will receive strong pain medicine intravenously and by injection during and after surgery, upon discharge your pain can be managed by oral pain medications. Some patients may not need narcotic pain medications within a few weeks of surgery
A small number of patients may require a blood transfusion depending on their blood counts, which are determined in the hospital after surgery.
Postoperative care:
Reverse Total Shoulder Replacement: Post-Operative Guidelines
Reverse Total Shoulder Replacement with Latissimus Transfer: Post-Operative Guidelines
You will meet with physical and occupational therapists in the hospital, and then visit with these specialists as an outpatient within the first 2-6 weeks after surgery. Your surgeon’s office will make these arrangements. Shoulder range of motion exercises will generally begin within the few first weeks after surgery, and strengthening exercises are initiated between 8-12 weeks after surgery. You will meet with your surgeon and care team several times in the first few months after surgery to ensure you are progressing appropriately.
You should plan to protect the arm for several weeks after the surgery, which means that help may be needed with daily chores, transportation, and other activities of daily living. Plan ahead for assistance from a friend, family member, or professional caregiver.
We typically recommend routine follow-up with your primary surgeon on a yearly or at least every other year basis.
A variety of patients may qualify for reverse total shoulder arthroplasty. As discussed above, the most common indication is a patient over 70 years old who has shoulder arthritis and a non-functioning rotator cuff. The reverse prosthesis, on rare occasions, may be used in relatively younger patients as a salvage procedure when no other feasible option exists for pain relief and functional improvement. The reverse prosthesis is considered a “salvage procedure” for younger, high demand patients because some limitations are indefinitely placed on the shoulder.For all patients, it is recommended to not use the operative arm for high demand activities such as heavy lifting, carpentry, chopping wood, or contact and collision sports. We generally recommend patients not perform strenuous activities with their arm, particularly with the reverse prosthesis to prevent early failure due to overuse. Obeying activity restrictions ensures increased longevity of the reverse prosthesis. Activities such as golf; however, seem to be well tolerated. (see testimonials)
A functioning deltoid muscle is required for a patient to undergo and gain benefit from a reverse prosthesis. Patients with nerve damage (particularly axillary nerve damage) or those with prior surgery complicated by a non-functioning deltoid muscle are not candidates for a reverse shoulder replacement.Additionally, patients with bone loss to their glenoids (or “socket”) may not be candidates for a reverse prosthesis because the implant cannot be fixed to native bone. This can happen when multiple prior surgeries cause significant bone loss or if a patient has severely abnormal bone anatomy of their shoulder.
Finally, patients with active infections are not candidates for a reverse prosthesis. Patients may undergo a reverse prosthesis only after an infection has been completely eradicated, typically a few months after having an antibiotic implant placed into their shoulder.

Figure 7: The picture demonstrates an example of a Prostalac antibiotic spacer.
Limited studies have shown partial shoulder replacements to have benefit for patients with arthritis and a non-functioning rotator cuff or in patients with failed prior shoulder replacements. These partial replacements are typically reserved for patients with poor bone quality of the glenoid, or “socket”, and in situations with failure of a prior prosthesis where a reverse is not possible.
Figure 8: The picture demonstrates an example of a hemiarthroplasty. The native glenoid remains while the proximal humerus has been replaced by a prosthetic device.
A final alternative to this procedure is the complete removal of the shoulder joint all together. This is known as a “resection arthroplasty” and is used as a final resort when all prior options have failed. This operation is rarely performed.

Figure 9: The picture shows an example of a resection arthroplasty. You can see that a screw remains in the scapular body after a failed reverse total shoulder arthroplasty and the ball of the shoulder joint has been removed.
Select articles on reverse shoulder replacements
