Proximal Humerus Fracture
Tim Hartshorn, M.D., Paul Yannopoulos, B.A., JJP Warner, MD (1/16/13)
The shoulder joint is made up of two bones, the scapula, which is also referred to commonly as the “shoulder blade,” and the humerus, which is the long bone in the arm. The joint is sometimes referred to as a “ball and socket” joint. The “socket” is a part of the scapula and is referred to as the glenoid. The “ball” comes from the upper part of the arm bone, the head of the humerus.
Figure: This normal shoulder xray shows the humeral shaft (arm bone), scapula (wing bone), and the proximal humerus (ball) which forms the shoulder joint by contacting the socket (glenoid)
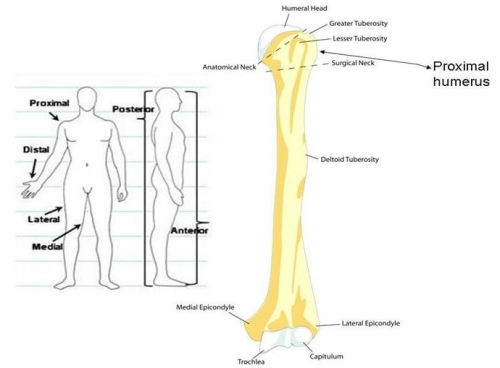
The word “proximal” is derived from the Latin proximus, which means nearest. When we use the word proximal to describe a portion of the human body, it means nearer to the center of the body. The opposite would be at the end of an extremity which is described as “distal”. In the case of the humerus bone, the “proximal” portion is the ball which is adjacent to the glenoid socket of the shoulder. The other end of the bone near the elbow is farther from the center of the body, so it is termed the “distal humerus.” (See figure below)
Fig: From The Vitruvian Man (drawing by Leonardo da Vinci circa 1487)
Figure below: The image to the left shows terminology used by physicians to explain proximal and distal as well as lateral and medial and anterior and posterior. The image to the right shows the anatomy of the humerus bone.
The word “fracture” means that the bone has a crack or break in it. This usually happens as the result of a fall or an accident.
A fracture of the proximal humerus means that the bone adjacent to the glenoid socket of the shoulder is broken (see below)
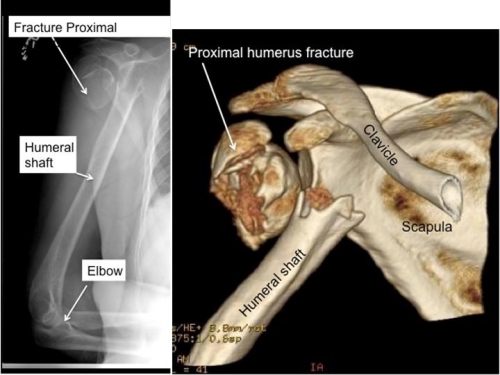
Figure: The image on the left is an x-ray of a proximal humerus fracture. The image on the right is a CT scan of a proximal humerus fracture
How Do Proximal humerus fractures occur?
Proximal humerus fractures almost always occur as the consequence of a fall or a significant trauma such as an automobile accident. In older individuals where the bone may be thin it may take less force for the proximal humerus to fracture.
Younger people generally have stronger bones that will not break with a simple fall. To break strong bones a larger amount of energy is required, like a car or motorcycle accident or a fall from a great height.

(http://www.cycling360media.com/crashing/)
Figure: This is an example of how a proximal humerus fracture may occur as the individual is about to land on his arm and shoulder.
X-rays show bones, not ligaments, arteries and other soft tissue such as tendons. (See figures below).
Figure: These are examples of proximal humerus fractures. An x-ray may help the treating orthopaedist to determine the type of proximal humerus fracture and the treatment necessary in each individual patient.
Proximal humerus fractures are generally defined by the quality of the bone, the number of parts to the fracture, and the extent of comminution. Comminution means many broken segments or pieces. The concept of “parts” is described and illustrated below and it is important to the decision for whether surgery is the best approach and if so which kind of surgery is most appropriate.There are potentially four parts of the proximal humerus (Neer CS, 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. The Journal of bone and joint surgery American volume. 1970;52(6):1077-89. Epub 1970/09/01.). The ball is one part, the greater tuberosity (attachment of part of the rotator cuff) is a second part, the lesser tuberosity (attachment of another part of the rotator cuff) is the third part, and the humeral shaft is the fourth part.
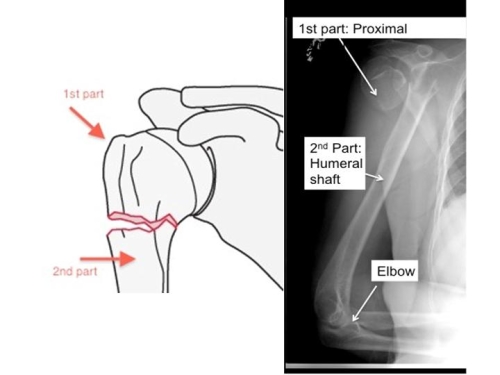
Figure: A two part fracture means that the proximal humerus is separated from the humeral shaft
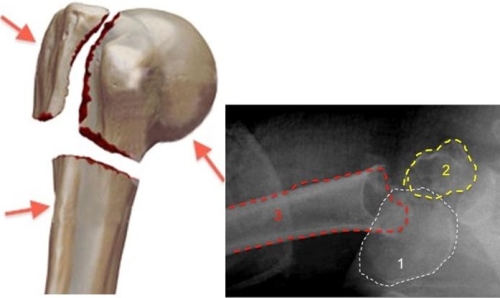
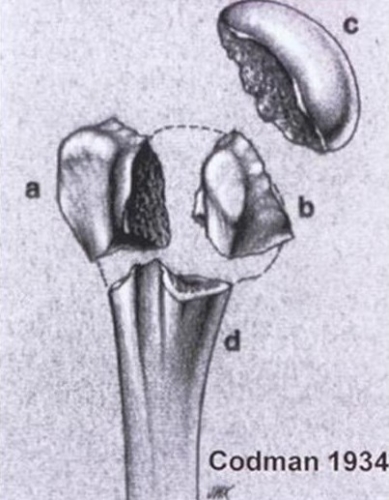
Figure. Image on the top, left: Three part proximal humerus fracture. The three different parts are indicated by the arrows. Image on the right: Three different parts are labeled. The Humeral head is 1. The Greater tuberosity is 2, and the humeral shaft is 3.
Figure: Codman described the Four Part concept of Humerus Fractures as shown above. A = greater tuberosity, B = lesser tuberosity, C = humeral head, D = humeral shaft
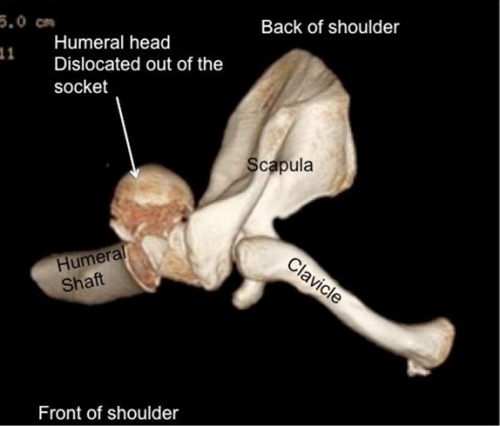
Figure: This is a 3-dimensional reconstruction of a CT scan showing a fracture-dislocation. In this case the humeral head is dislocated out of the socket and into the back of the shoulder
The quality of the bone is important as an important factor for determining the potential for repair of the fracture. Older individuals have thin bone which appears to be porous (see figure below). As we age our bone becomes thinner and more porous and thus is weaker. This is termed osteoporosis.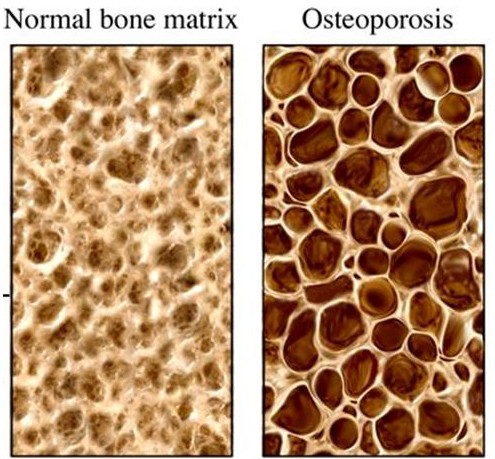
Figure: This is a microscopic view of bone of the proximal humerus. Normal bone is more dense (see on the left) versus osteoporotic bone which appears more porous (see on the right). (Figure from whatisosteoporosis.net)
Another important issue is that the bone of the humeral head (ball) has a blood supply and this may be damaged when the bone fractures. This is usually more of a risk with more complex fractures such as a 3-part or 4-part fracture or a fracture dislocation. A problem which may come from this injury is called avascular necrosis. This means the bone losses a blood supply and the ball may eventually collapse leading to arthritis (link to AVN module) This condition may take years to develop (See figure below)

Figure: The humeral head has collapsed (white arrows) due to loss of blood supply after a fracture. This is called avascular necrosis . Image on left shows view from front (anterior-posterior view) and image on right shows view from underneath arm (axillary view).
Non-operative treatment is selected when the fracture is only minimally displaced or in some cases where surgery would be expected to have a greater risk than non-operative treatment due to the bone quality or factors related to the patient. Some patients may not be well suited to surgery due to their overall health or ability to comply with the necessary aftercare following surgery. Moreover, their bone quality may be poor and attempted surgical fixation might fail due to the poor holding power of the bone.In cases where the bones are minimally displaced healing without surgery will usually result in good function (see figure below).
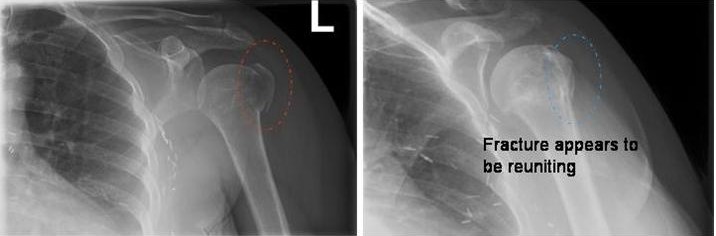
Left image: Initial xray at time of fracture; Right image:The fracture has healed six months later.

Figure: The patient above is the one shown in the x-rays of the minimally displaced fracture above. Note the excellent motion six months after the fracture injury.
Non-operative treatment: The injured arm is usually placed into a shoulder immobilizer for 2-4 weeks. Physical therapy which usually begins when the sling is removed, involves gentle stretching of the shoulder to restore motion. After a few months strengthening may begin.
When the extent of fracture displacement makes it unlikely non-operative treatment will result in a good functional outcome, surgery may be recommended. If the bone fragments are of good quality then open reduction of the pieces of the fracture and fixation is the best treatment option. In some cases the pieces of the fracture may be manipulated through small incisions under x-ray control and fixed with pins. Most of the time open repair with plate and screws and strong sutures is required. (See figure below)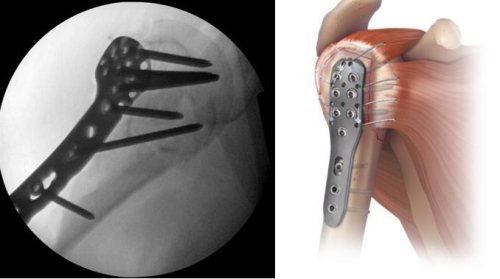
Figure: A variety of special plates allow for fixation of the fracture once the broken pieces are moved into position. Usually x-ray control is used during surgery to guide the repair process (see image to the upper left).
Hemiarthroplasty
In some cases the bone is broken so badly that repair is not possible. In such a case replacement of the broken proximal humerus with an artificial ball and stem (hemiarthroplasty) is indicated. (See figures below)
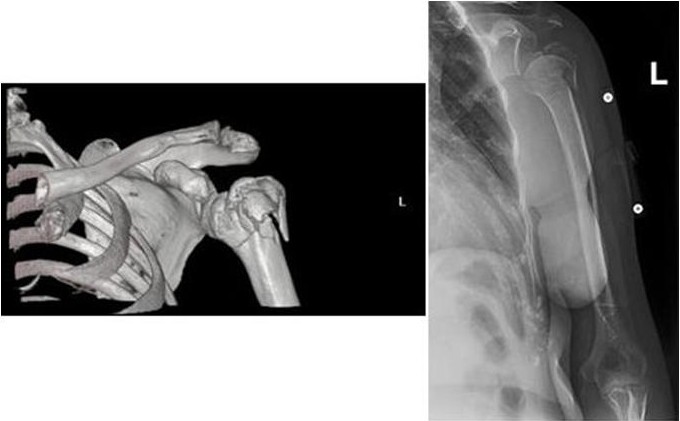
Figure: The images above show an elderly patient with a proximal humerus fracture where the bone is in many pieces (comminuted) and thus not well suited to a fracture repair.
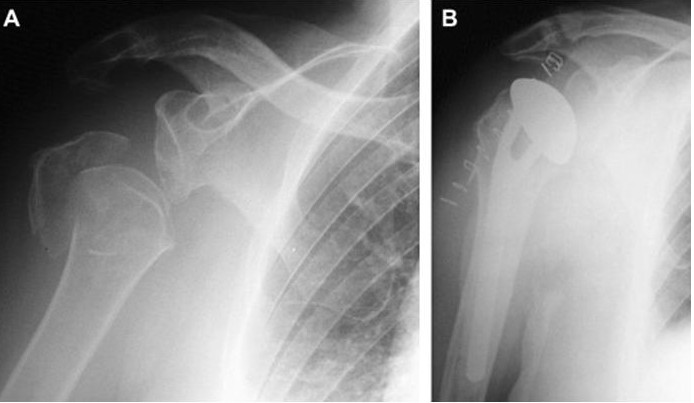
Figure:A) X-ray showing proximal humerus fracture B) X-ray after placement of a hemiarthroplasty
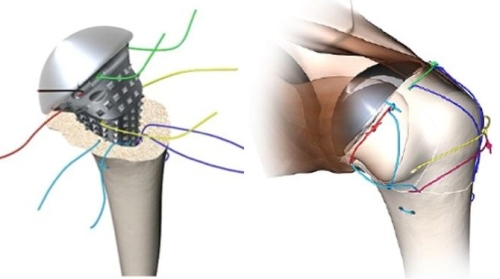

Figure: Placement of the hemiarthroplasty requires methodical repair of tuberosity fragments which are attached to the rotator cuff tendons (upper two figures). During the surgery x-ray with a fluoroscopy until guides the surgeon (lower left image). The postoperative x-ray is shown in the lower right image.

Figure: This patient is one year after replacement of her fractured shoulder with a hemiarthroplasty.
In elderly individuals with poor quality bone (osteoporosis) and marked comminution (many fragments) even hemiarthroplasty is unlikely to give a good functional outcome as the bony fragments are not likely to heal around the hemiarthroplasty. In such cases a reverse prosthesis allows for better shoulder function (Link to Reverse Module).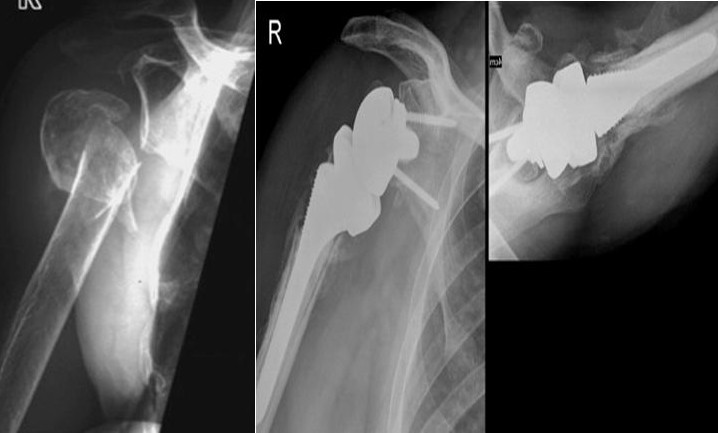

Figure: Severe (comminuted) proximal humerus fracture in a 74 year old woman (upper left). A reverse prosthesis has been performed (upper right). One year after surgery function is excellent (lower two images). (Case courtesy of C. Gerber, M.D.)
Reverse Total Shoulder Replacement: Our Experience
Reverse Total Shoulder Replacement: Post-Operative Guidelines
Reverse Total Shoulder Replacement with Latissimus Transfer: Post-Operative Guidelines
Proximal humerus fractures account for 4-5% of all adult fractures. In patients aged older than 65, they represent the third most common fracture behind hip and distal radius fractures.4 The management options for proximal humerus fractures has expanded in recent years, and patients with displaced, unstable proximal humerus fractures may have improved outcomes if managed operatively. Interobserver agreement between surgeons in the treatment of proximal humerus fractures is moderate overall, and further outcomes research to establish if the choice of treatment actually influences the clinical outcome.3 Current data that is used to assist in the decision making process are discussed below.Non-operative treatment has been the mainstay of treatment for non-or minimally displaced proximal humerus fractures. In a retrospective study by Zyto, 15 patients with a 3 or 4-part proximal humerus fracture were evaluated at a minimum follow-up of 10 years, and the mean constant score was 59 and 47 respectively with a mean flexion and abduction over 90 degrees. Only 4 patients reported pain and it was graded as mild. In spite of low functional scoring and poor fracture reduction in many shoulders, the patient’s contentment with their injured shoulder remained high at 10 years.6 In another recent randomized controlled trial studying older patients with a displaced four-part fracture of the proximal humerus, hemiarthroplasty improved health related quality of life but not functional outcome more than nonoperative treatment did.5
When looking at the literature, we can also get some general numbers on how well people do when treated surgically for these types of fractures. In 1970, Dr. Charles Neer, one of the pioneers of modern shoulder surgery, noted generally poor outcomes of displaced 3 and 4-part proximal humerus fractures. He concluded that humeral head replacement was the treatment of choice for these fractures, thus shaping treatment algorithms that are still used today.1,2
Besch et al.8 assessed the clinical outcomes of 34 patients with four-part fractures treated with hemiarthroplasty. Eighteen patients were treated with primary hemiarthroplasty, and 16 underwent hemiarthroplasty after failed initial ORIF. The authors noted better clinical outcomes and a lower incidence of tuberosity malalignment in those patients treated with primary hemiarthroplasty. Hemiarthroplasty serves as a viable option for pain relief in persons with displaced 3 and 4-part fractures. In a systematic review, Kontakis et al.10 reported on 810 hemiarthroplasties that were followed for an average of 3.7 years from surgery. Most of these fractures were 4-part fractures or fracture-dislocations. On average, patients had 106 degrees of forward flexion (arm out to the front), 92.4 degrees of abduction (arm out to the side), and 30 degrees of external rotation (shoulder rotating out). Complications related to tuberosity healing were observed in 11.2% of cases, heterotopic ossification in 8.8% of cases, and proximal migration of the humeral head in 6.8% of cases. At the final follow-up, no pain or only mild pain was experienced by most patients, but marked limitation of function persisted.
Solberg et al.9 compared hemiarthroplasty with ORIF using a locked-plate construct in patients with 3 or 4-part proximal humerus fractures. In this retrospective study involving 122 patients 55 years or older with an average of 36 months follow-up, the authors found better Constant shoulder scores in the group treated with ORIF versus hemiarthroplasty (68.6 versus 60.6, respectively). Complications of ORIF in this study included avascular necrosis in 6 patients, screw perforation of the humeral head in six patients, loss of fixation in four patients, and a wound infection in three patients. Complications of the hemiarthroplasty group included nonunion of the tuberosity in seven patients and wound infection in three patients.
Although a technically demanding procedure, the use of a reverse prosthesis (RSA) is sometimes the better choice for some older patients. Gallinet et al.11 looked at 40 patients with complex 3 and 4-part proximal humerus fractures. Nineteen underwent RTSA and 21 received a hemiarthroplasty. After 12.4 and 16.5 months of follow-up, respectively, Constant scores (53 versus 39), active abduction (91° versus 60°), and active forward elevation (97.5° versus 53.5°) were higher in the RTSA group compared to the hemiarthroplasty group. Rotation was better in the hemiarthroplasty group however (external rotation 13.5° versus 9°, internal rotation 55° versus 31°). Thus, a reverse prosthesis can provide a reliable, rapid, and predictable result in terms of abduction, anterior elevation and pain relief, but impaired rotation.
Overall, there is insufficient evidence in the literature to dictate exactly how proximal humerus fractures should be managed. In a meta-analysis of twenty-three small, randomized controlled trials between 2001-2012 pertinent to the management of proximal humerus fractures in adults, Handoll et al.7 made the following conclusions:
1. Early physiotherapy, without immobilization may be sufficient for some types of non-displaced fractures.
2. It is unclear whether surgery, even for specific fracture types, will produce consistently better long-term outcomes but is it likely to be associated with a higher risk of surgery-related complications and requirement for further surgery.
3. There is insufficient evidence to establish what is the best method of surgical treatment in terms of the use of different categories (such as plate versus hemiarthroplasty)
4. There is insufficient evidence to say when to start mobilization after either ORIF or hemiarthroplasty.
References
1. Neer CS, 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. The Journal of bone and joint surgery American volume. 1970;52(6):1077-89. Epub 1970/09/01.
2. Neer CS, 2nd. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. The Journal of bone and joint surgery American volume. 1970;52(6):1090-103. Epub 1970/09/01.
