Shoulder Arthritis Including Joint Replacement
(Xinning “Tiger” Li, M.D.; Paul Yannopoulos, B.A.; Jon JP Warner, M.D.) Dec. 2012. Printable Version: Shoulder Arthritis Including Joint Replacement Module
Click here for more information on: “Trial without Error: The Value of Virtual Surgery”
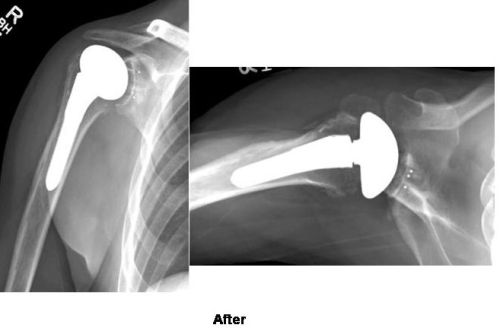
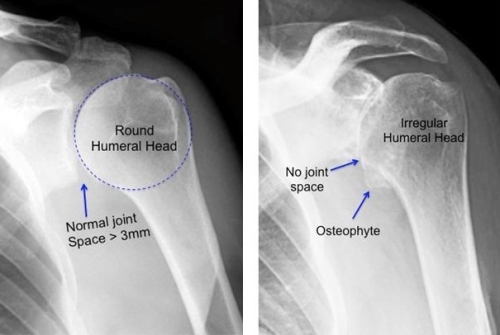 Figure: The normal shoulder joint is a round ball on a concave socket (image on left) and the normal cartilage joint space is 3mm or greater. In arthritis the joint space is narrowed and the humeral head (ball) becomes irregular and flattened (image on right).The shoulder complex is made up of three bones: Scapula(shoulder blade), humerus (upper arm bone), and theclavicle (collarbone). The shoulder joint (glenohumeral joint) is composed of the humeral head of the upper arm bone (ball) and the glenoid socket, which is the outer part of the shoulder blade. Unlike the other large ball-in-socket joint in the body, the hip, the shoulder joint is a ball-on-socket. And the humeral head (ball) is larger than the socket (glenoid). This allows for the wide range of motion required for overhead sports and work.
Figure: The normal shoulder joint is a round ball on a concave socket (image on left) and the normal cartilage joint space is 3mm or greater. In arthritis the joint space is narrowed and the humeral head (ball) becomes irregular and flattened (image on right).The shoulder complex is made up of three bones: Scapula(shoulder blade), humerus (upper arm bone), and theclavicle (collarbone). The shoulder joint (glenohumeral joint) is composed of the humeral head of the upper arm bone (ball) and the glenoid socket, which is the outer part of the shoulder blade. Unlike the other large ball-in-socket joint in the body, the hip, the shoulder joint is a ball-on-socket. And the humeral head (ball) is larger than the socket (glenoid). This allows for the wide range of motion required for overhead sports and work. As with all joints, movement is permitted by smooth, slippery cartilage surfaces which allow for minimum friction when the joint moves. This joint surface appears as white and shiny. An xray of a normal shoulder appears as a dark joint space of 3 mm or greater and this is the normal cartilage thickness of the shoulder joint (see above). The shoulder joint is stabilized by ligaments and muscles. The muscles of the rotator cuff also help move the ball on the socket. The normal joint cartilage is a thin shiny surface of about 2mm in thickness (see diagram below)
As with all joints, movement is permitted by smooth, slippery cartilage surfaces which allow for minimum friction when the joint moves. This joint surface appears as white and shiny. An xray of a normal shoulder appears as a dark joint space of 3 mm or greater and this is the normal cartilage thickness of the shoulder joint (see above). The shoulder joint is stabilized by ligaments and muscles. The muscles of the rotator cuff also help move the ball on the socket. The normal joint cartilage is a thin shiny surface of about 2mm in thickness (see diagram below) 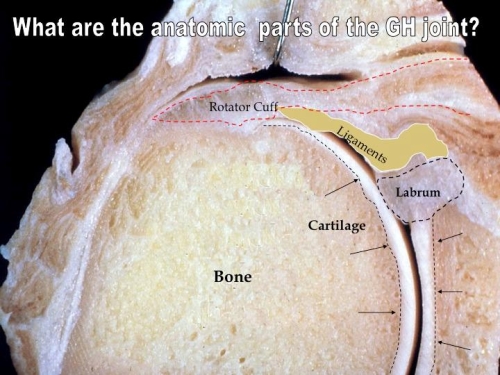 A normal shoulder joint allows you to throw, swim, work overhead, weight-lift and perform other similar activities. Unfortunately, as a result of trauma, wear and tear, and other processes, arthritis can develop.
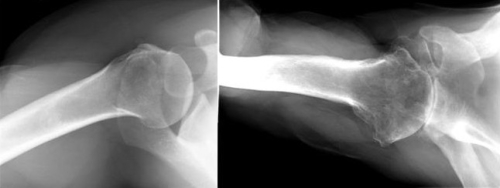
A normal shoulder joint allows you to throw, swim, work overhead, weight-lift and perform other similar activities. Unfortunately, as a result of trauma, wear and tear, and other processes, arthritis can develop. 2) Post-traumatic arthritis of the shoulder results when the shoulder joint is injured. This can be a result of bone fracture, dislocation, or damage to the surrounding ligaments/soft tissue around the shoulder joint. This is a 22-year-old woman with arthritis after a fracture skiing and a surgical repair (screws and plate have been removed). Note that the humeral head (ball) is irregular and flattened.
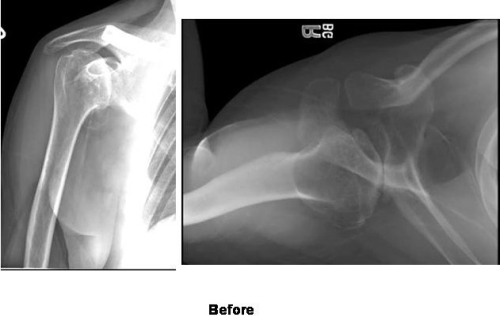
2) Post-traumatic arthritis of the shoulder results when the shoulder joint is injured. This can be a result of bone fracture, dislocation, or damage to the surrounding ligaments/soft tissue around the shoulder joint. This is a 22-year-old woman with arthritis after a fracture skiing and a surgical repair (screws and plate have been removed). Note that the humeral head (ball) is irregular and flattened. 
 3) Rheumatoid Arthritis and other inflammatory conditions of the shoulder is a systemic disease that can affect any joint in the body. This is a condition in which the lining of the joint (synovial cells) develops inflammation which damages the cartilage and bone of the shoulder. In some cases it is inherited and a family history of rheumatoid arthritis may be a cause. Women are affected more frequently than men and sometimes young adults can develop a form of this called juvenile rheumatoid arthritis. Typically, other joints are also affected such as the hands, knees, and even the spine.Your physician may order blood tests which show markers for this inflammatory condition. This condition is different than typical osteoarthritis, as the process often results in erosions of the bone around the joint, and the rotator cuff tendons may also be damaged. In some cases, bony erosions and tendon damage may be severe. The lower image shows a severe loss of tendons and erosion of bone that has caused the humeral head to move upward out of the socket.
3) Rheumatoid Arthritis and other inflammatory conditions of the shoulder is a systemic disease that can affect any joint in the body. This is a condition in which the lining of the joint (synovial cells) develops inflammation which damages the cartilage and bone of the shoulder. In some cases it is inherited and a family history of rheumatoid arthritis may be a cause. Women are affected more frequently than men and sometimes young adults can develop a form of this called juvenile rheumatoid arthritis. Typically, other joints are also affected such as the hands, knees, and even the spine.Your physician may order blood tests which show markers for this inflammatory condition. This condition is different than typical osteoarthritis, as the process often results in erosions of the bone around the joint, and the rotator cuff tendons may also be damaged. In some cases, bony erosions and tendon damage may be severe. The lower image shows a severe loss of tendons and erosion of bone that has caused the humeral head to move upward out of the socket. 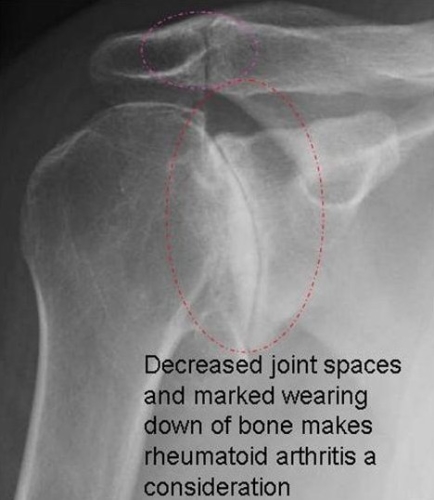
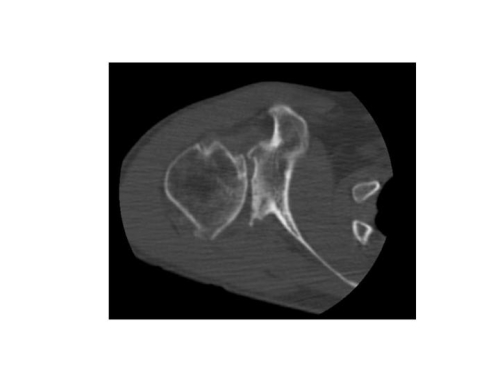
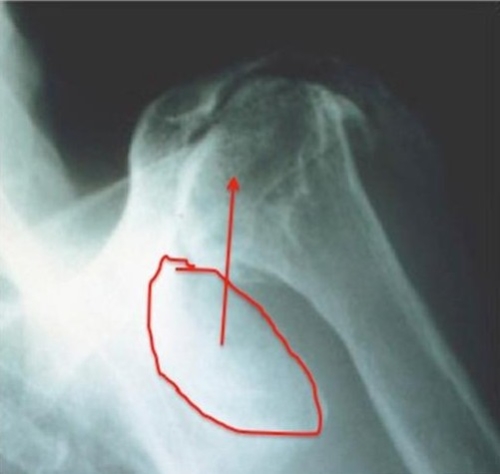 Other Causes: Arthritis can occur after surgery as when anchors for an instability repair are placed in a location to damage the joint cartilage. The patient’s XRays below shows anchors placed in a location that damaged the joint cartilage. This patient developed arthritis as the result of metal anchors placed into the joint surface during a surgery to treat recurrent shoulder instability. The joint is irregular and there are erosions of the glenoid (socket).
Other Causes: Arthritis can occur after surgery as when anchors for an instability repair are placed in a location to damage the joint cartilage. The patient’s XRays below shows anchors placed in a location that damaged the joint cartilage. This patient developed arthritis as the result of metal anchors placed into the joint surface during a surgery to treat recurrent shoulder instability. The joint is irregular and there are erosions of the glenoid (socket). 
 The joint is irregular and there are erosions of the glenoid (socket). See CT image below.
The joint is irregular and there are erosions of the glenoid (socket). See CT image below. 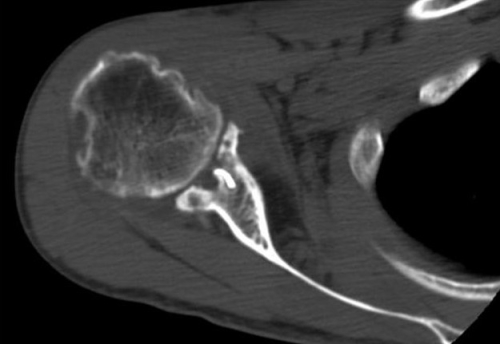 Sometimes arthritis can occur after over tightening of the joint with instability surgery. This may result in loss of motion and damage to the joint surfaces over many years.
Sometimes arthritis can occur after over tightening of the joint with instability surgery. This may result in loss of motion and damage to the joint surfaces over many years. 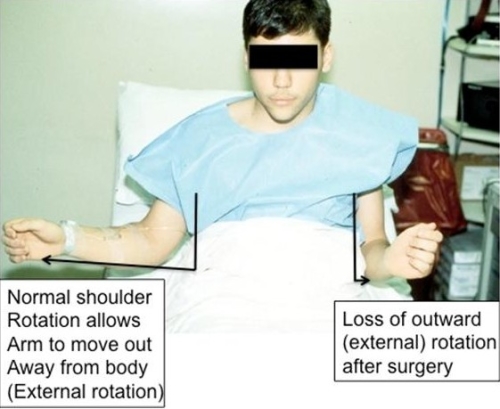
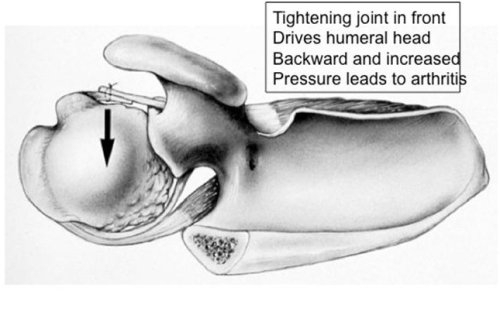
 Figures above: Sometimes shoulder instability surgery may result in over-tightening of the joint and loss of external rotation (movement of the arm out to the side). (Top figure). The result of this over-tightening can be the development of arthritis, as the humeral head (ball) is pushed out the back of the joint and overloads the cartilage which then degenerates (lower two images). Other causes of shoulder arthritis that may affect younger patients include: Humeral head avascular necrosis, iatrogenic causes, chondrolysis (may be result of pain pumps, infection, application of heat during surgery), post surgery arthritis, etc. Avascular necrosis is a condition where the humeral head blood supply (which is critical in healthy bone maintenance) is disrupted and causes bone death. The bone collapses over time and will result in arthritis.
Figures above: Sometimes shoulder instability surgery may result in over-tightening of the joint and loss of external rotation (movement of the arm out to the side). (Top figure). The result of this over-tightening can be the development of arthritis, as the humeral head (ball) is pushed out the back of the joint and overloads the cartilage which then degenerates (lower two images). Other causes of shoulder arthritis that may affect younger patients include: Humeral head avascular necrosis, iatrogenic causes, chondrolysis (may be result of pain pumps, infection, application of heat during surgery), post surgery arthritis, etc. Avascular necrosis is a condition where the humeral head blood supply (which is critical in healthy bone maintenance) is disrupted and causes bone death. The bone collapses over time and will result in arthritis. 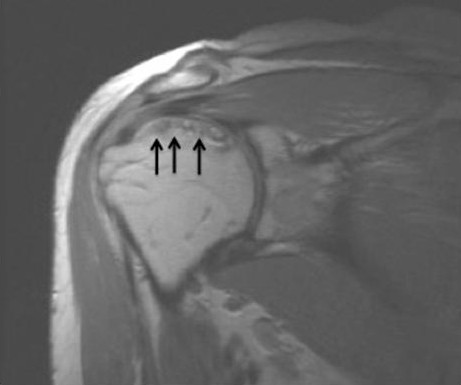
 (Above left: AVN with collapse of superior-upper humeral head after loss of blood supply to bone-arrows; Above right: Severe AVN with flattening of humeral head after a fracture) Arthritis after surgery may be due to overtightening of a joint with instability surgery (see above), damage from implants and anchors for repair of tendons and ligaments (see above), infection, or simply unexplained. Chondrolysis is a condition characterized by rapid loss of cartilage in the shoulder joint. It has been associated with the use of intraarticular pain pumps, infection, application of heat with devices which are used to shrink tissue in shoulder stabilization operations, insertion of absorbable anchors, or simply with no known cause. It typically affects young and active adults and can be devastating in terms of its effect on quality of life. Rarely, congenital (from birth) deformities of the joint can lead to earlier arthritis than is typically seen in osteoarthritis form from wear and tear. See figure below:
(Above left: AVN with collapse of superior-upper humeral head after loss of blood supply to bone-arrows; Above right: Severe AVN with flattening of humeral head after a fracture) Arthritis after surgery may be due to overtightening of a joint with instability surgery (see above), damage from implants and anchors for repair of tendons and ligaments (see above), infection, or simply unexplained. Chondrolysis is a condition characterized by rapid loss of cartilage in the shoulder joint. It has been associated with the use of intraarticular pain pumps, infection, application of heat with devices which are used to shrink tissue in shoulder stabilization operations, insertion of absorbable anchors, or simply with no known cause. It typically affects young and active adults and can be devastating in terms of its effect on quality of life. Rarely, congenital (from birth) deformities of the joint can lead to earlier arthritis than is typically seen in osteoarthritis form from wear and tear. See figure below:  Figure: 40 year old woman with severe joint deformity and underdeveloped, small glenoid socket as the result of dwarfism.
Figure: 40 year old woman with severe joint deformity and underdeveloped, small glenoid socket as the result of dwarfism.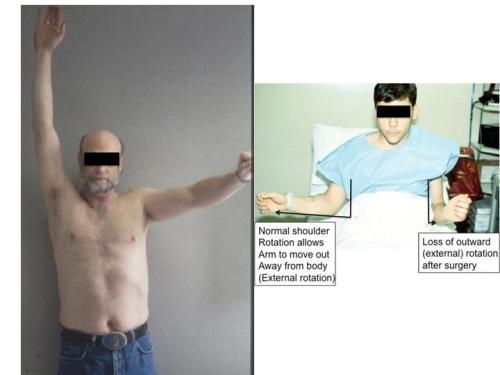
A history of progressive loss of motion and pain interfering with sports, work, and eventually daily activities is a typical complaint of patients. Loss of sleep due to pain is also and important complaint we typically hear from patients. Crunching (crepitation), grinding sensations, and catching may also be symptoms the patient notices. You may also notice noise or crunching (crepitation) in your shoulder. Weakness maybe present simply due to pain interfering with your ability to move your arm.The examination by a shoulder specialist will demonstrate loss of active motion but also passive motion. This is true stiffness as a result of the arthritic process and joint deformity which develops. Strength may be affected due to pain but is usually not true weakness.
Radiographs or X-Rays
Routine X-Rays will be ordered in the anteroposterior (AP) and axillary views. 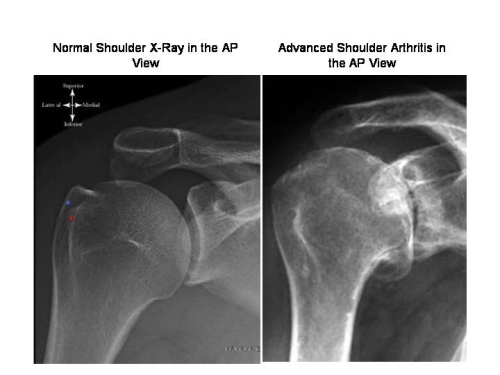
MRI or CT Scan
Additional imaging may include a CAT Scan and sometimes an MRI. Many surgeons use a CAT scan to see the extent of joint deformity and help them plan for the shoulder reconstruction once surgery is elected by the patient. An MRI does not provide much useful information about the joint but can be helpful if there is a question about the rotator cuff in a patient who might also have weakness.
CT:
MRI:
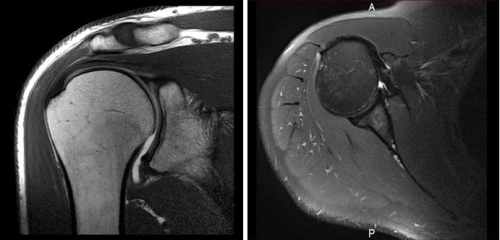 Fig. MRI is usually only useful in patients who may have an associated rotator cuff tendon tear as it is not particulary accurate for cartilage loss and bony deficiencies. http://www.bosshin.com/rotator_cuff_pathologies/
Fig. MRI is usually only useful in patients who may have an associated rotator cuff tendon tear as it is not particulary accurate for cartilage loss and bony deficiencies. http://www.bosshin.com/rotator_cuff_pathologies/
 Joint supplementation with glucosamine/chondroitin can also be use to treat arthritis. Glucosamine and chondroitin (G/C) are two molecules that make up the cartilage found in your shoulder joint. They are the building blocks for cartilage formation. The theory of using glucosamine and chondroitin is that by congestion of more building blocks then there is more available for cartilage regeneration. However, there is currently no scientific evidence proving that the consumption of glucosamine and chondroitin will increase the quantity and also quality of the articular cartilage in an arthritis shoulder joint. There are many studies done in the literature on the use of G/C in arthritis. Most of these studies are done in patients with knee or hip arthritis. There is evidence that using G/C supplementation will have more pain relief than placebo, however, no studies in the literature have shown that using G/C will alter the natural history of arthritis.
Joint supplementation with glucosamine/chondroitin can also be use to treat arthritis. Glucosamine and chondroitin (G/C) are two molecules that make up the cartilage found in your shoulder joint. They are the building blocks for cartilage formation. The theory of using glucosamine and chondroitin is that by congestion of more building blocks then there is more available for cartilage regeneration. However, there is currently no scientific evidence proving that the consumption of glucosamine and chondroitin will increase the quantity and also quality of the articular cartilage in an arthritis shoulder joint. There are many studies done in the literature on the use of G/C in arthritis. Most of these studies are done in patients with knee or hip arthritis. There is evidence that using G/C supplementation will have more pain relief than placebo, however, no studies in the literature have shown that using G/C will alter the natural history of arthritis.  Cortisone injection is another alternative method of treatment in patients with arthritis. Typically the cortisone is injected in combination with another pain reducing medication into your shoulder joint under imaging guidance. Cortisone is a type of anti-inflammatory medication and it helps to reduce the inflammation as it is directly injected into your shoulder joint. Injections of corticosteroids may give marked pain relief; however, this effect is usually limited and may last anywhere from a few hours to a few months. Repeated such injections raises the risk for infection or damaging effects of steroid to the rotator cuff tendons.
Cortisone injection is another alternative method of treatment in patients with arthritis. Typically the cortisone is injected in combination with another pain reducing medication into your shoulder joint under imaging guidance. Cortisone is a type of anti-inflammatory medication and it helps to reduce the inflammation as it is directly injected into your shoulder joint. Injections of corticosteroids may give marked pain relief; however, this effect is usually limited and may last anywhere from a few hours to a few months. Repeated such injections raises the risk for infection or damaging effects of steroid to the rotator cuff tendons.  Other alternatives include injection of joint lubrications fluid (Synvisc-TM, Orthovisc-TM , Hyalgan-TM, etc) into the shoulder. This is basically artificial joint fluid with the proposed mechanism being protective by reducing joint compression and friction. There may also be an anti-inflammatory effect. The majority of the studies done with these injection are in the knee and hip joint, and some have shown at least a temporary relief of pain similar to corticosteroid injections. The use of such injections for the shoulder has been limited (literature?) with no evidence of a reproducible effect or benefit above corticosteroid injection. In addition, insurance companies will generally not cover the expense of such an injection.
Other alternatives include injection of joint lubrications fluid (Synvisc-TM, Orthovisc-TM , Hyalgan-TM, etc) into the shoulder. This is basically artificial joint fluid with the proposed mechanism being protective by reducing joint compression and friction. There may also be an anti-inflammatory effect. The majority of the studies done with these injection are in the knee and hip joint, and some have shown at least a temporary relief of pain similar to corticosteroid injections. The use of such injections for the shoulder has been limited (literature?) with no evidence of a reproducible effect or benefit above corticosteroid injection. In addition, insurance companies will generally not cover the expense of such an injection. 
Total Shoulder Replacement Post-Operative Protocol
Article/abstract on patient expectations after TSA:
Henn RF 3rd, Ghomrawi H, Rutledge JR, Mazumdar M, Mancuso CA, Marx RG. J Bone Joint Surg Am. Preoperative patient expectations of total shoulder arthroplasty. 2011 Nov 16;93(22):2110-5. 98 patients underwent TSA at HSS were evaluated with preoperative evaluation included the American Shoulder and Elbow Surgeons (ASES) score, Shoulder Activity Scale, Short Form-36 (SF-36), and visual analog scale scores for shoulder pain, fatigue, and general health. Expectations were evaluated with use of the Hospital for Special Surgery’s Shoulder Surgery Expectations Survey. Expectations were not associated with education, history of previous joint replacement, or comorbidities. However, younger patients had greater expectations of TSA which resulted in worse general health on the visual analog scale and worse ASES scores.  There are many different brands of shoulder replacement implants. While all may differ in some design features they all attempt to help the surgeon achieve the same goal: Pain relief and improved function from patient. This is accomplished by allowing modularity of the components to fit different sizes patients with different joint deformities and to attempt to restore normal anatomy. There is no evidence that one design is better than another while changes in design features and even bearing surfaces are ongoing.
There are many different brands of shoulder replacement implants. While all may differ in some design features they all attempt to help the surgeon achieve the same goal: Pain relief and improved function from patient. This is accomplished by allowing modularity of the components to fit different sizes patients with different joint deformities and to attempt to restore normal anatomy. There is no evidence that one design is better than another while changes in design features and even bearing surfaces are ongoing.
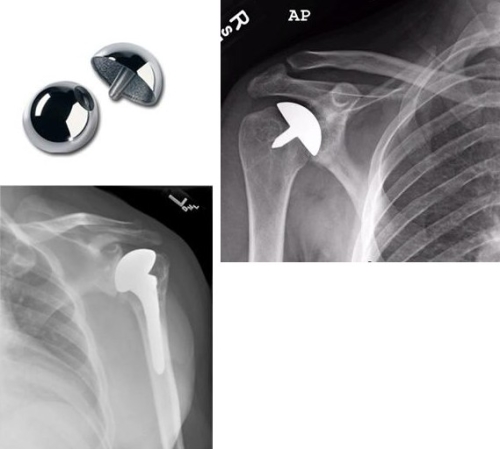
 Case Example 1: 22 Year old skier with posttraumatic arthritis after a fracture skiing. This was treated with a hemiarthroplasty. 4 years later she has no pain and is very active in sports.
Case Example 1: 22 Year old skier with posttraumatic arthritis after a fracture skiing. This was treated with a hemiarthroplasty. 4 years later she has no pain and is very active in sports. 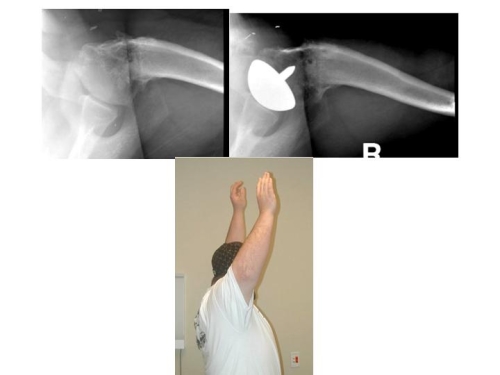 Case 2: 19 year old mechanic with limited motion and pain due to a severe joint deformity from birth and after a failed surgery. He had a resurfacing and four years later is working as a mechanic with no pain.
Case 2: 19 year old mechanic with limited motion and pain due to a severe joint deformity from birth and after a failed surgery. He had a resurfacing and four years later is working as a mechanic with no pain.Understanding Total Shoulder Replacement: A Patient Guide