Clavicle (Collar Bone) Fractures
Matthew F. Dilisio, MD; Tamara Pylawka, MD, MS; and Jon J.P. Warner, MD (8/5/2013)
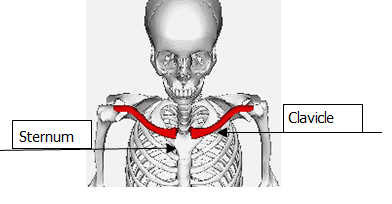
The collar bone (or clavicle) is the bone that runs along the front of the shoulder to the breast bone (sternum). The clavicle is an “S” shaped bone that is subcutaneous its entire length. The middle third of the clavicle protects important structures underneath it (brachial plexus and axillary artery). The clavicle plays an important role in abduction (raising the arm) and adduction (lowering the arm) power of the upper extremity. It is also critical to overhead activity during overhead use of the upper extremity.
Clavicle fractures are often caused by a direct hit to the shoulder. This can happen during a fall onto the shoulder or a car collision. A fall with the arm outstretched to help brace a fall can also cause a clavicle fracture. Mechanisms of injury have been reported by Robinson et al. and include simple fall, fall from height, sport injury, motor vehicle accidents and violence. (JBJS Br 1998; 80:476-‐84). Injuries associated with clavicle fractures include nerve injury (brachial plexus), rib fractures, vascular injuries, lung injury and other skeletal injury (AC and SC separation or fracture-‐dislocation).


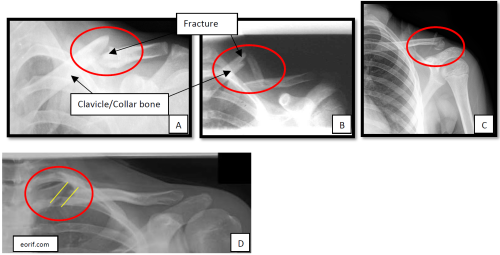
Types of clavicle fractures and what do Xray images of clavicle fractures look like?
Clavicle fractures can be simple as shown in the mid-shaft fracture above (A). These fractures can also be complex with multiple fragments. The image above (B) shows a free segment of the clavicle due to two breaks. This is characterized as a butterfly fragment. The location of the fracture may also be important as in image (C), showing a fracture of the lateral (outer) end of the bone which also involves the acromioclavicular (AC) joint. The most rare fracture type is a medial clavicle fracture as seen in image (D).
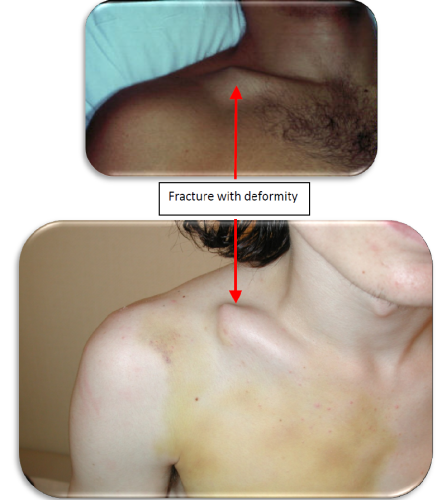
When a patient sustains a clavicle fracture this is usually associated with severe pain and bruising. There may also be a deformity or asymmetry of the shoulder due to the movement of the clavicle fracture fragments. The shoulder may appear shorter than the other side and it may droop downward; and there may also be swelling from bleeding (hematoma). This swelling will resolve and bruising will also go away over several weeks. There will usually be pain when you try to move your arm and you may hear or feel crunching (crepitation) which is actually the movement of the ends of the fracture.
Clavicle fractures have been reported to represent 2.6% of all fractures (Postacchini et al.). Nordqvist and Petersson have reported the incidence of clavicle fracture to be 64 per 100,000 fractures per year. Recent evidence based studies by Zlowodzki and McKee et al. have been designed to offer treatment options for the most common clavicle fracture type: midshaft fractures (http://www.ncbi.nlm.nih.gov/pubmed/18310682). Briefly the results of this study suggested that when a fracture has a lot of displacement it is recommended to do operative fixation of these fractures. The results indicated better functional outcomes and a decreased rate of the complication of healing in the wrong position (malunion) or not healing at all (non-union).
Clavicle fractures can be treated non-operatively or operatively depending on the type of fracture. Fractures that do not have a lot of displacement or many pieces can be treated with no surgery. Fractures that are very displaced, damaging the skin, puncturing the skin, or having many pieces may need surgery to help them heal correctly. Fractures in the distal end of the clavicle may interfere with the AV (acromioclavicular) joint and may need operative treatment.
Operative treatment is absolutely indicated if the fracture is open (penetration through the skin), the skin is under tension, and if the skin is at risk of breakdown (see below image). Relative indications include a patient with multiple traumatic injuries, seizure disorder, or floating shoulder. Recent literature also has concluded that operative indications include 100% displacement of the fracture fragments, 2 cm of shortening (overlap of the fractures) or comminution (many pieces) of the fracture.
Operative and non-operative treatment methods exist for treatment of mid-shaft clavicle fractures. These fractures are always operated on if they are open or the bone punctures the skin. When these fractures are closed, the treatment modalities are discussed with patients. When fractures of the clavicle are minimally displaced, then close follow-up with repeat x-rays and non-operative treatment is recommended. If the fracture has multiple pieces or has a large amount of displacement, then a decision between operative and non-operative treatment will be discussed, as treatment is still controversial with studies suggesting better outcomes with operative intervention.
A recent prospective study by McKee and Altamimi examined the patient outcomes and complication rates following non-operative or operative (plate fixation) of displaced mid-shaft clavicle fractures. Conclusions of their study included that operative fixation resulted in improved function of the upper extremity and lower rates of nonunion and malunion at one year of follow-up. Most complications were reported in the operative group and included skin irritation secondary to hardware prominence, wound infection, and plate failure. (http://www.ncbi.nlm.nih.gov/pubmed/18310682).
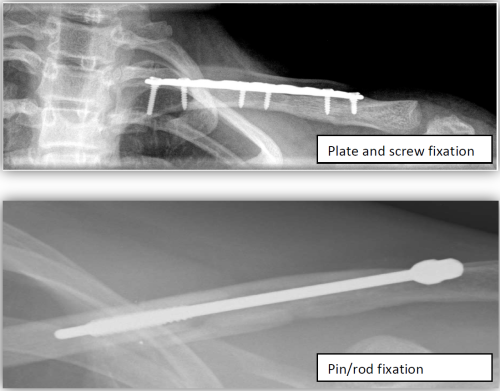
When operative treatment is decided by the patient and physician most middle clavicle fractures can be treated with a plate/screws or with a intramedullary rod although no clear evidence exists on which operative fixation is better.
At the Boston Shoulder Institute, we recently published our results comparing plating versus intramedullary rod fixation for clavicle fractures. Kleweno et al. reviewed 40 consecutive patients with simple (wedge shape) and closed mid-shaft clavicle fractures. Pin/rod implants were used in 18 patients and plates were used in 14 patients. All patients with intramedullary rod placement had complete healing of the fracture and all had planned rod removal. In the patients that had plating of their fractures, slow healing (delayed union) occurred in one patient and 2 patients had re-fractures. Our conclusion was that both procedures are safe and predictable to treat acute mid-shaft clavicle fractures.(http://www.ncbi.nlm.nih.gov/pubmed/21723149).
Is the hardware (plates and/or screws) retained or removed?
Hardware is always removed when the fracture is fixed using a pin/rod construct. The pin is used as a temporary device to hold the fracture in the correct alignment while healing occurs. When a plate is used the hardware is sometimes removed if prominence of the plate is not tolerated by the patient.
Hill et al. reported on complications associated with non-operative treatment (JBJS (Br), 1997):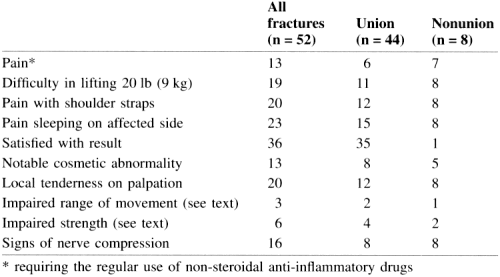
Complications include infection, hardware failure, non-union, mal-union, and re-fracture after hardware is removed.
Zlowodzki et al. (JOT 19:504-7) reported that non-union (fracture does not heal) of displaced fracture treated non-operatively were 15% and treated operatively with plates were 2.2%. When using a pin/rod, the non-union rate was 2.0%.
Bostman et al. reported on complications of plate fixation in displaced mid-shaft clavicle fractures. This study included 103 adult fractures that were displaced middle third fractures treated with plate fixation. In their group, 23% had one or several of the following complications: deep infection, plate breakage, nonunion, or refracture after plate removal. Their infection rate was 7.8%.
Shen et al. reported their complications on operative outcomes of 251 displaced clavicle fractures with complications including 7 patients (3%) nonunion, 28 patients with some sense of numbness over the incision site and above the incision site, and a deep infection in 1 patient. No patients in this group were reported to have loss of motion or shoulder strength. Overall, 94% of patients were satisfied with the procedure.
The purpose of surgery is to align the fracture fragments and hold them together rigidly so that the bone cells (osteoblasts) can make new bone which heals the fracture. Thus, the fixation with the plate andscrews, pin, or sutures acts as a temporary internal stabilization while the bone heals. In general it takes about 4 weeks for the bone to heal sufficiently to allow for active motion of the arm, so you will be in a sling for this period of time. Your surgeon may have you do passive motion with a physical therapist moving your arm for you in order to avoid stiffness. Below are links to examples of passive range of motion exercises:
- Pendulum Hangs
- Sitting Assisted Forward Reach
- Doorway Standing External Rotation
- Sidelying Internal Rotation Stretch at 70 Degrees
After 4 weeks (or longer if your surgeon deems this to be necessary) the sling will be removed and you will be permitted and encouraged to use your arm for daily living activities such as washing, dressing, and when comfortable, driving. Periodic radiographs over the weeks after surgery will allow your surgeon to judge healing and decide when strengthening may begin (usually around 3 months after surgery). Below are links to examples of some of these more advanced physical therapy exercises:
- Active Range of Motion Forward Flexion in the Scapular Plane
- Active Range of Motion External Rotation with Band Strengthening
- Active Range of Motion Internal Rotation with Band Strengthening
- Lateral Clavicle Fractures: Lateral clavicle fractures constitute 15% of all clavicle fractures. Neer classified these fractures depending on the relationship of the fracture line to the acromialclavicular (AC) joint and the coracoclavicular (CC) ligaments. Type I is characterized by minimal displacement (interligamentous between the AC joint and CC ligaments). Type II is characterized by displacement of the fracture secondary to fracture medial to CC ligaments. Type III involves the joint and is considered intra‐articular fracture.
- Type I: minimal displacement (between AC and CC)

- Type II: Displaced 2 degrees to fracture medial to CC ligaments

- Type III: Intra-articular fracture
- Type I: minimal displacement (between AC and CC)
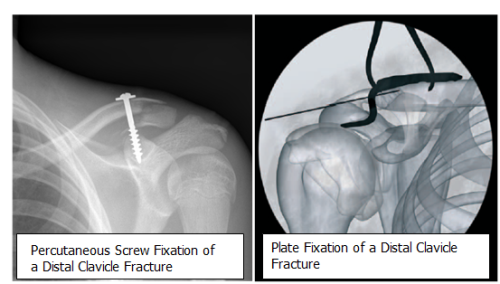
Treatment options for distal clavicle fractures depend on the type of fracture.
Type I fractures are considered stable because the CC ligament is intact and prevents fracture fragments from displacement. For this fracture a sling is used to support the arm and gradual motion is started with pendulum activity. The sling can be removed with the pain is lessened and activity is gradually advanced with strengthening started once pain free shoulder range of motion occurs.
Type II factures are more involved and can be further subdivided as those fractures that occure medial to the CC ligament and those that occur lateral to the CC ligament. These fractures are unstable and have a high non‐ union rate (30%). Nordqvist et al. found 10 non‐unions out of 23 type II fractures. Edwards et al. reported up to 75% patients with type II fractures treated non‐surgically developed a delayed union or nonunion. Rokito et al. reported nonunion in 7 of 16 patients treated non‐surgically for type II fractures. Robinson et al reported on clinical assessment of patients with distal clavicle non‐unions and found that 14% were eventually symptomatic and needed later surgical reconstruction.
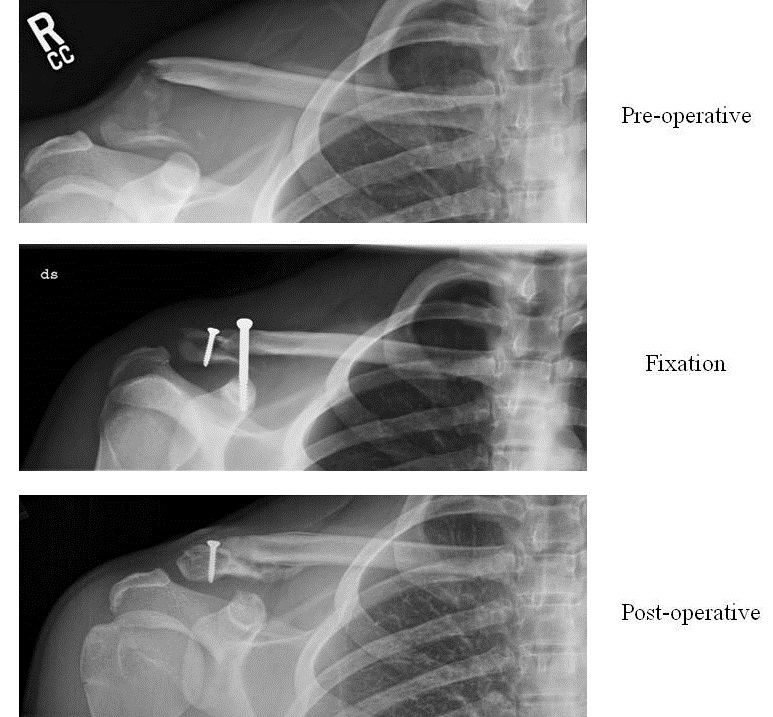
Given this high rate of non‐union, many clinicians are proponenets of operative intervention for type II distal clavicle fractures. Fractures that have marked displacement, open fractures, and fractures threatening the overlying skin are clearly indications for surgery. There are multiple methodsto fix distal clavicle fractures with no one technique superior. They include wires, pins, plates, sutures and a coraclavicular screw.
- Postoperative Care of Lateral Clavicle: Post operative care will include sling for comfort. Post op check (10‐14 days post op) includes assessment of the wound and to starting gentle passive range‐of‐motion (ROM). At 6 weeks, xrays are obtained and if union is evident then gradual strengthening is started. At 3 months, repeat films are taken and if patient is pain free and bone is healed then the patients are released to full activity.
- Complications of Non-Operative Care of Lateral Clavicle FracturesThere is generally a 30% risk of non‐union (failure of the fracture to heal) will non‐operative care. If a non‐union develops, patients can be minimally symptomatic with little loss of function. If a symptomatic non‐unions occurs, then a late reconstructive surgical option are available.Type III lateral clavicle fractures that are treated non‐operatively have higher risk of developing AC joint arthritis. However, a study by Nordquist et al. noted no long‐term problems at 15 year follow‐up for this type of fracture. Nonoperative treatment for this type of fracture involves a sling that is used to support the arm and gradual motion is started with pendulum exercises. The sling can be removed with the pain is lessened and activity is gradually advanced with strengthening started once pain free shoulder range of motion occurs.
Distal Clavicle Fracture Case Example
References:
- Robinson CM. Fractures of the clavicle in the adult. Epidemimiology and classification. J Bone Joint Surg Br. 1998 May; 80(3):476-84.
- Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002 Sep-Oct;11(5):452-6.
- Nordqvist A, Petersson CJ. Incidence and causes of shoulder girdle injuries in an urban population. J Shoulder Elbow Surg. 1995 Mar‐Apr;4(2):107‐12.
- Altamimi SA, McKee MD; Canadian Orthopaedic Trauma Society. Nonoperativetreatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J Bone Joint Surg Am. 2008 Mar;90 Suppl 2 Pt 1:1‐8.
- Kleweno CP, Jawa A, Wells JH, O’Brien TG, Higgins LD, Harris MB, Warner JJ.Midshaft clavicular fractures: comparison of intramedullary pin and plate fixation. J Shoulder Elbow Surg. 2011 Oct;20(7):1114‐7.
- Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle‐third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997 Jul;79(4):537‐9
- Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD; Evidence‐Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence‐ Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005 Aug;19(7):504‐7.
- Böstman O, Manninen M, Pihlajamäki H. Complications of plate fixation in freshdisplaced midclavicular fractures. J Trauma. 1997 Nov;43(5):778‐83.
- Shen WJ, Liu TJ, Shen YS. Plate fixation of fresh displaced midshaft clavicle fractures. Injury. 1999 Sep;30(7):497‐ 500.
- Nordqvist A, Petersson C, Redlund‐Johnell I. The natural course of lateral clavicle fracture. 15 (11‐21) year follow‐up of 110 cases. Acta Orthop Scand.1993 Feb;64(1):87‐91.
- Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distalclavicle: a case for fixation. Injury. 1992;23(1):44‐ 6.
- Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA. Acomparison of nonoperative and operative treatment of type II distal claviclefractures. Bull Hosp Jt Dis. 2002‐2003;61(1‐2):32‐9.
- Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateralfractures of the clavicle. J Bone Joint Surg Am. 2004 Apr;86‐A(4):778‐82.