2023 Outcomes Report (Dr. Lohre)
One of the core values of our service is measurement and transparency. Thus, every year we review all surgical cases performed by physicians on our service and report these publicly for prospective and current patients to review as they wish. This is a short-term review as we perform longer-term analysis for publication and for cohort reporting for all patients separate from this report. By measuring outcomes, we can analyze our treatment in order to continually improve care.
Dr. Lohre’s outcomes data is collected and compiled by the clinical research coordinator for the service, utilizing the electronic medical records system of Massachusetts General Hospital as well as surgical billing data. Our methodology consists of a review of all operations performed during the calendar year on a case-by-case basis, with special consideration made to procedure type, patient past surgical history (primary vs. revision status), and any complications arising during or after an operation. This data was collected, aggregated, and independently analyzed by the research coordinator with no direct input from the attending physician. The final review was performed by the surgeon in order to check accuracy of procedures and outcomes.
2023 Surgical Overview
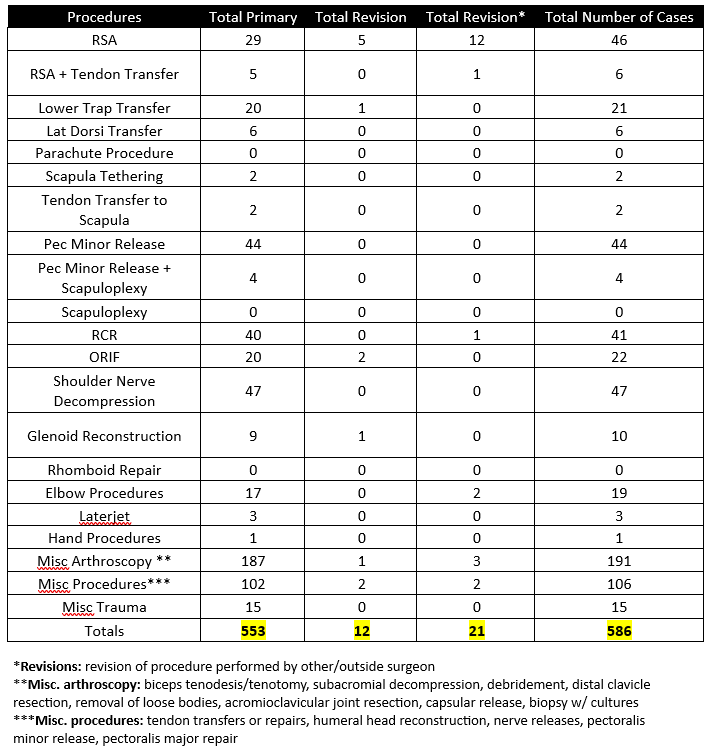
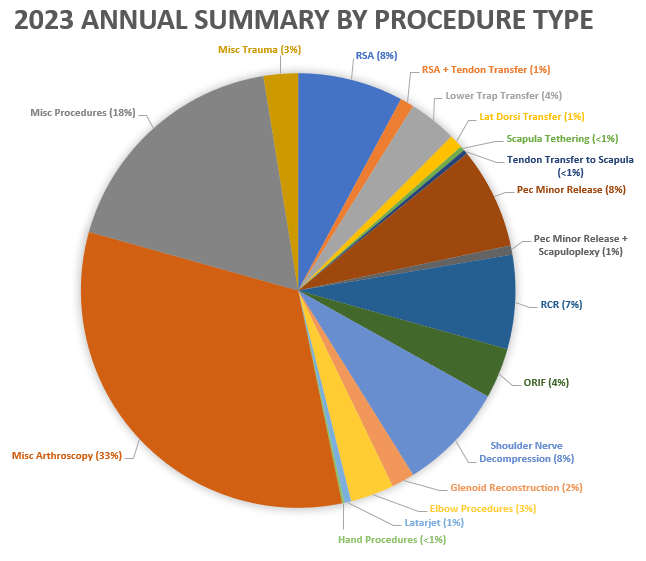
The following section will provide an overview of all cases done by Dr. Lohre in 2023. Importantly, procedures are not the same as total surgeries performed – one surgery may (and often does) include multiple procedures completed during the same operation. For example, a patient may undergo a shoulder arthroplasty and a biceps tendon tenodesis during the same surgery. These are recorded below as separate procedures, but as a single surgery.
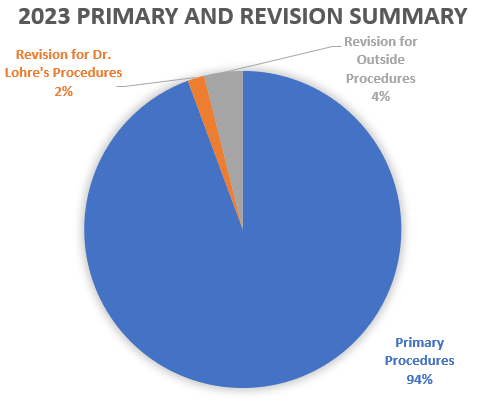
- 586 procedures were performed on 241 patients by Dr. Lohre during the 2023 calendar year.
- Of these 586 procedures, 553 were primary procedures. A “primary” procedure refers to the first surgical intervention done for a patient’s condition. If Dr. Lohre performs a rotator cuff repair on a patient who has not had a repair done on that shoulder yet, this would be considered a primary surgery. 12 of these procedures were revisions of his own past cases (these revisions were performed in 2023, but the primary procedure was done at a prior time time). 21 of these procedures were revisions of procedures performed by other/outside surgeons
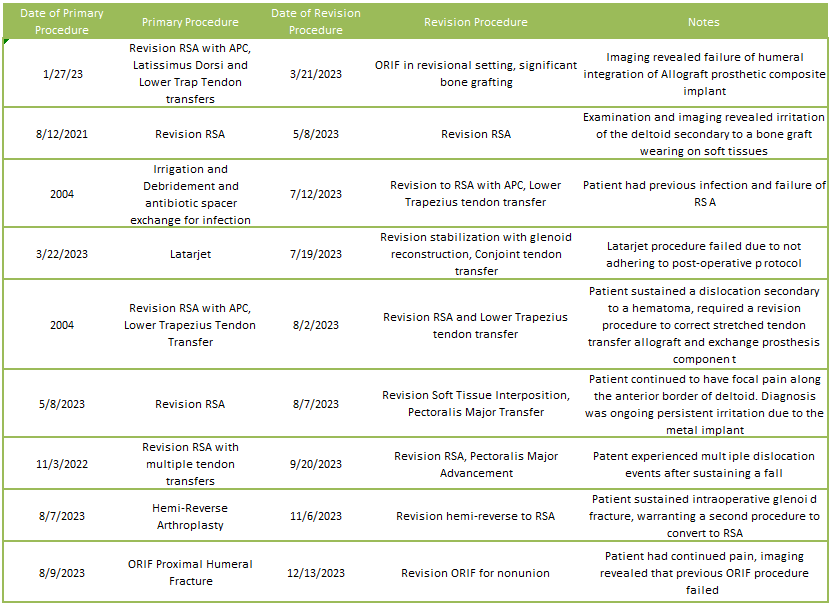
2023 Revision Descriptions
Of the 6% of Dr. Lohre’s 2023 cases that were revisions, the average interval between primary and revision surgery was about 6.4 years. The shortest interval was 53 days, and the longest interval was 350 months or about 29 years. These revision procedures are summarized below:
2023 Revisions for Outside Cases
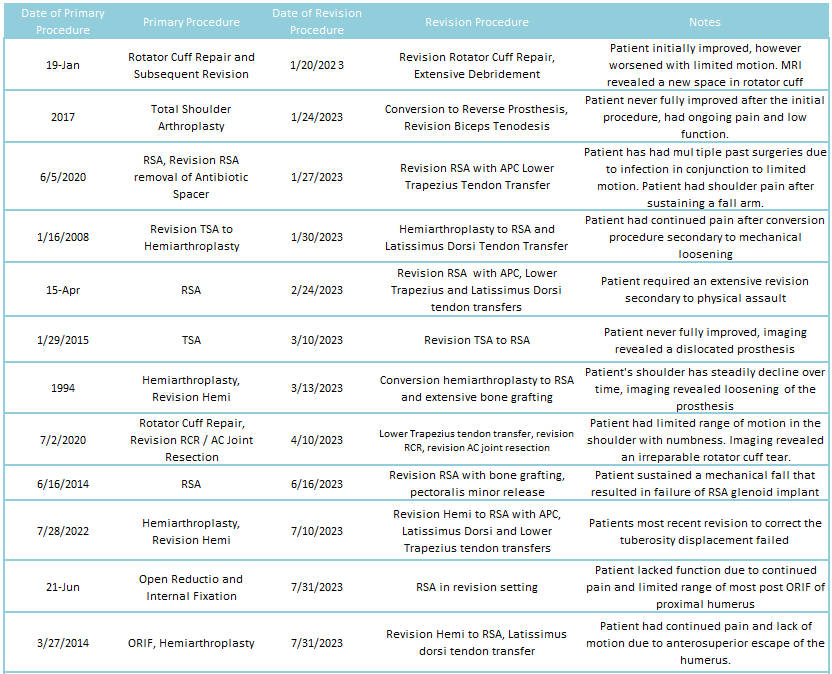
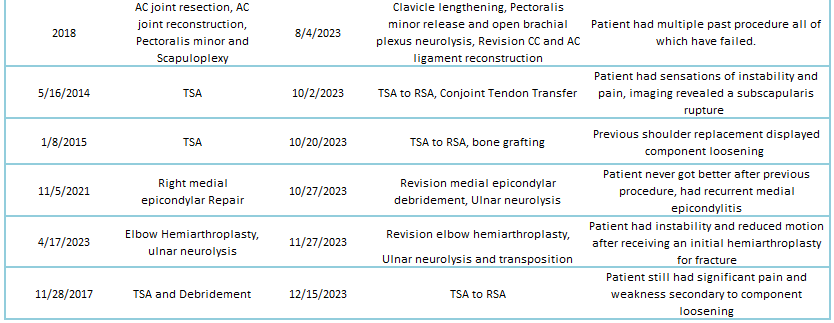
2023 Revisions for Dr. Lohre’s Cases
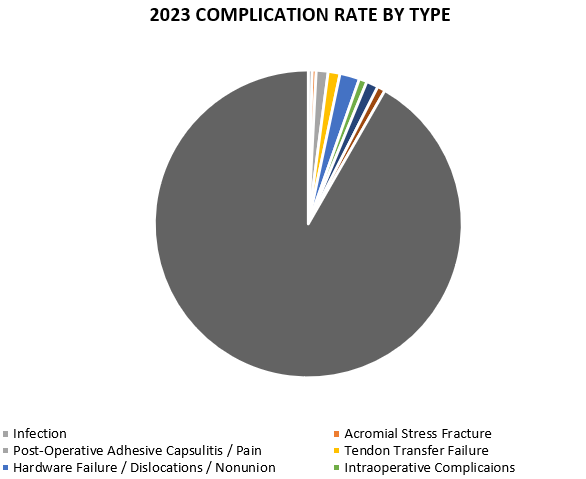
2023 Complications Overview
Of 241 patients operated on by Dr. Lohre in 2023, 20 patients (8.3%) experienced a complication during or after surgery. These complications were identified in 2023. Of the 20 complications, 10 required additional surgeries, while the overall reoperation rate was 4.1% (10 reoperations out of 241 patients operated). An explanation of each complication can be found below. Items in green were patients who had resolution of their complication and those indicated in red had an ongoing issue at the time of this reporting.
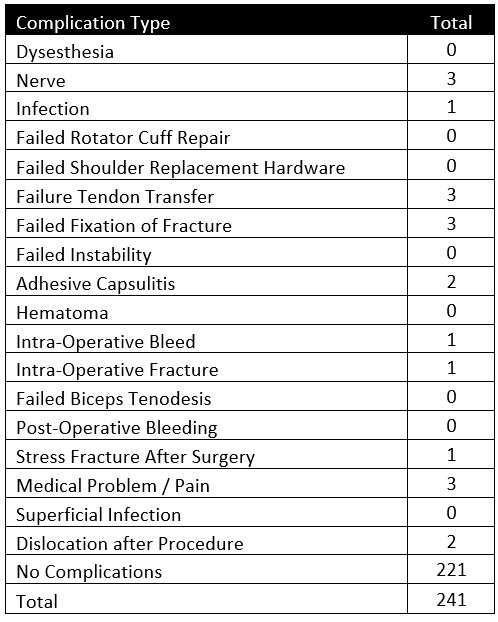
Infection
This patient experience symptoms of infection post Reverse Shoulder Arthroplasty and underwent a subsequent Irrigation and Debridement. The patient continued to have drainage required a second surgery to address a periprosthetic infection. The patient is doing much better with no signs of infection.
Acromial Stress Fracture
This patient experienced pain after Reverse Shoulder Arthroplasty and Latissimus Dorsi Tendon Transfer procedures. CT scanning revealed an acromial stress fracture. The patient was immobilized for 4 weeks and is much better, resuming sports.
Post-Operative Adhesive Capsulitis / Pain
This patient underwent a Rotator Cuff Repair procedure and developed stiffness secondary to adhesive capsulitis and irritation from spinal hardware. The patient saw minimal improvement with conservative treatment and injections. It was deemed no more surgical management for the shoulder was appropriate and the patient was referred to physiatry.
This patient underwent an Intermedullary Rodding Procedure to correct a fracture, experiencing pain and numbness around the elbow and inside portion of the forearm. Patient underwent subsequent Hardware Removal procedure with a Capsular Release with minimal improvement. Patient was indicated for a Reverse Shoulder Arthroplasty procedure.
This patient underwent a Lower Trapezius Tendon Transfer procedure and developed stiffness secondary to adhesive capsulitis. Although still having persistent stiffness, the patient indicated that it does not affect daily life. Patient was indicated for an arthroscopic capsular release, but the patient wishes to follow conservative treatments for now.
Tendon Transfer Failure
This patient post Reverse Shoulder Arthroplasty and Lower Trapezius Tendon Transfer procedures experienced a tendon transfer failure. Patient underwent subsequent revision Lower Trapezius Tendon Transfer procedure and is doing significantly better, restoring motion of the shoulder.
This patient underwent a Lower Trapezius Tendon Transfer that failed postoperatively. The patient underwent a subsequent Reverse Shoulder Arthroplasty procedure with a Latissimus Dorsi Tendon Transfer. The patient is doing much better and has full range of motion now.
This patient underwent a Lower Trapezius Tendon Transfer that failed postoperatively. The patient underwent a revision Lower Trapezius Tendon Transfer procedure. The patient had improved range of motion but experienced increased stiffness in the shoulder. Patient was indicated for a capsular release procedure to address stiffness.
Hardware Failure / Dislocations / Nonunion
This patient underwent a Posterior Glenoid Reconstruction procedure x-rays incomplete incorporation of bone graft and a failed screw. Patient underwent a subsequent revision Posterior Glenoid Reconstruction procedure to remove the broken screw. Patient is doing significantly better and was able to return to sports.
This patient underwent a Revision Reverse Shoulder Arthroplasty procedure and experience multiple atraumatic dislocation events. After examination, it was deemed that over stretched tissues caused these events. Patient was advised to stop activity and immobilize The patient is doing significantly better with no new dislocation events.
This patient underwent a revision Reverse Shoulder Arthroplasty procedure and Lower Trapezius Tendon Transfer, developing a significant hematoma, causing a dislocation and stretching of the tendon allograft. Patient underwent a subsequent revision Reverse Shoulder Arthroplasty and Tendon Transfer procedure to correct the dislocation. Patient does continue to have pain but is significantly better.
This patient underwent Open Reduction Internal Fixation procedure of the proximal humerus of which failed. The patient had a subsequent revision Open Reduction Internal Fixation and post-operatively developed axillary neuropathy. Patient was indicated for pinning and shoulder fusion surgeries to restore motion of the shoulder.
This patient after receiving a revision to Reverse Shoulder Arthroplasty procedure experienced significant pain and lack of range of motion postoperatively. Imaging revealed a nonunion of allograft utilized in the revision procedure. The patient was indicated for an additional revision Reverse Shoulder Arthroplasty, but the patient wished to treat her pain conservatively at this time.
Intraoperative Complications
This patient underwent a Reverse Shoulder Arthroplasty procedure and sustained an intraoperative bleed. The rest of the procedure went according to plan and the patient recovered well and is happy with their shoulder.
This patient was indicated for a Reverse Shoulder Arthroplasty procedure but received a Hemi-Reverse Arthroplasty due to an intraoperative fracture, warranting a second surgery to convert the shoulder to a Reverse Prosthesis. The patient did very well overall with some stiffness that was address with therapy.
Nerve Complications
This patient underwent a hardware removal surgery and developed significant pain post-operatively and was found to have axillary neuropathy in addition to known rotator cuff deficiency. Patient was in and stepped away from work. Patient was indicated for a Lower Trapezius Tendon Transfer procedure.
This patient underwent an Arthroscopic Pectoralis Minor Release without alleviation hand numbness that existed pre-operatively. Patient was diagnosed with Snapping Scapula syndrome and has been indicated for an additional procedure in Serratus Anterior advancement procedure to remediate symptoms.
This patient underwent a Reverse Shoulder Arthroplasty procedure and developed forearm numbness post-operatively secondary to intraoperative compressive neuropathy. The patient improved significantly better with time and no longer has numbness in the operative shoulder.
Other
This patient underwent a Pectoralis Major Transfer and developed a rash and secondary to an allergy to Nickel and Cobalt hardware. Patient was indicated for a subsequent revision Arthroplasty procedure to swap components with a Titanium prosthesis.
This patient underwent a revision Total Elbow Arthroplasty procedure and was unable to actively bend all fingers. Further testing ruled out nerve damage, and the patient was referred to the MGH Hand Service to remediate the lack of function in the hand. The patient is now significantly better and can bend all fingers.
