2024 Outcomes Report (Dr. Lohre)
One of the core values of our service is measurement and transparency. Thus, every year we review all surgical cases performed by physicians on our service and report these publicly for prospective and current patients to review as they wish. This is a short-term review as we perform longer-term analysis for publication and for cohort reporting for all patients separate from this report. By measuring outcomes, we can analyze our treatment in order to continually improve care.
Dr. Lohre’s outcomes data is collected and compiled by the clinical research coordinator for the service, utilizing the electronic medical records system of Massachusetts General Hospital as well as surgical billing data. Our methodology consists of a review of all operations performed during the calendar year on a case-by-case basis, with special consideration made to procedure type, patient past surgical history (primary vs. revision status), and any complications arising during or after an operation. This data was collected, aggregated, and independently analyzed by the research coordinator with no direct input from the attending physician. The final review was performed by the surgeon in order to check accuracy of procedures and outcomes.
2024 Surgical Overview
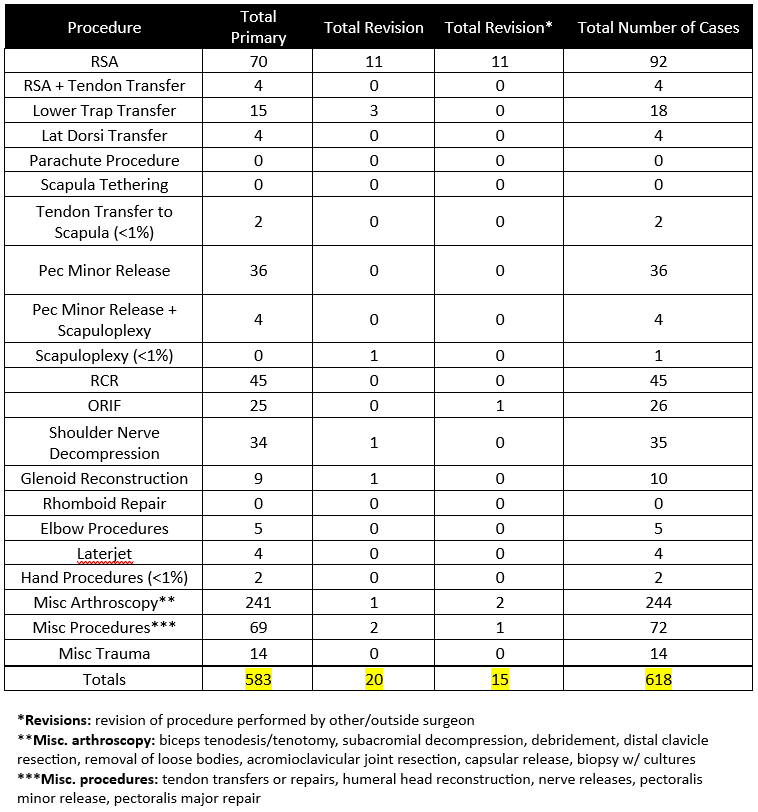
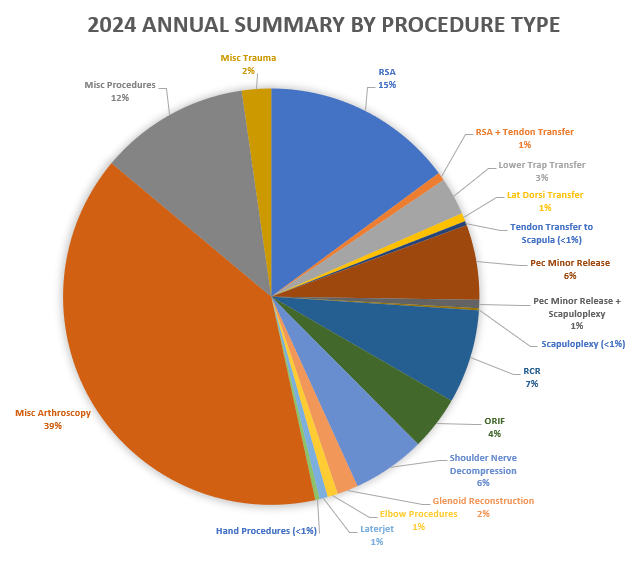
The following section will provide an overview of all cases done by Dr. Lohre in 2024. Importantly, procedures are not the same as total surgeries performed – one surgery may (and often does) include multiple procedures completed during the same operation. For example, a patient may undergo a shoulder arthroplasty and a biceps tendon tenodesis during the same surgery. These are recorded below as separate procedures, but as a single surgery.
- 618 procedures were performed on 280 patients by Dr. Lohre during the 2024 calendar year.
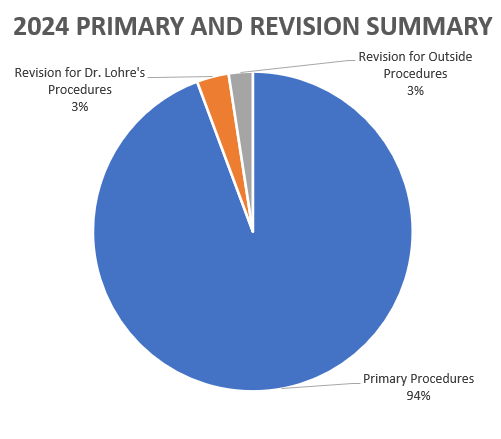
- Of these 586 procedures, 583 were primary procedures. A “primary” procedure refers to the first surgical intervention done for a patient’s condition. If Dr. Lohre performs a rotator cuff repair on a patient who has not had a repair done on that shoulder yet, this would be considered a primary surgery. 20 of these procedures were revisions of his own past cases (these revisions were performed in 2024, but the primary procedure was done at a prior time time). 15 of these procedures were revisions of procedures performed by other/outside surgeons
2024 Revision Descriptions
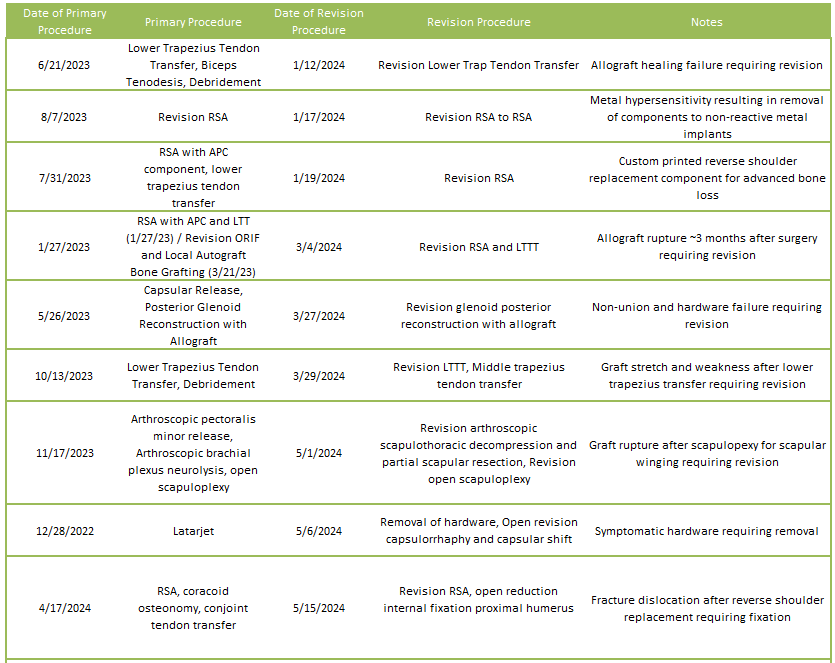
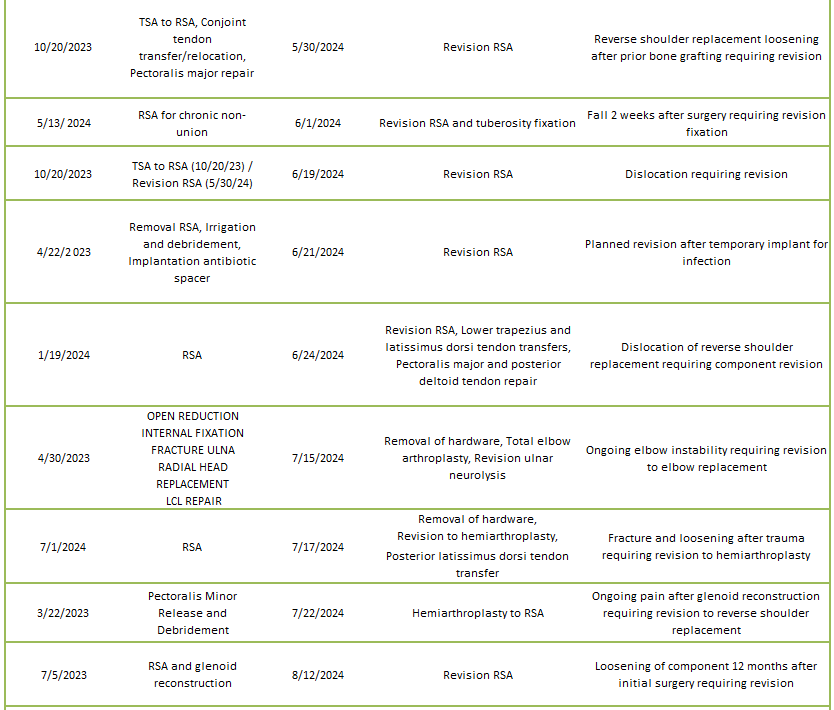
Of the 6% of Dr. Lohre’s 2024 cases that were revisions, the average interval between primary and revision surgery was about 2.0 years. The shortest interval was 16 days, and the longest interval was 128 months or about 10.7 years. These revision procedures are summarized below:
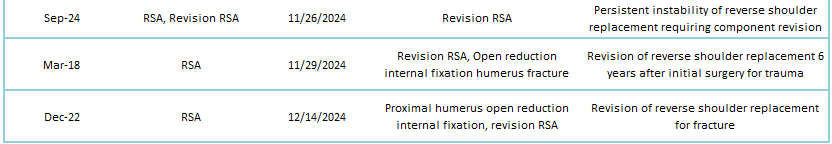
2024 Revisions for Outside Cases
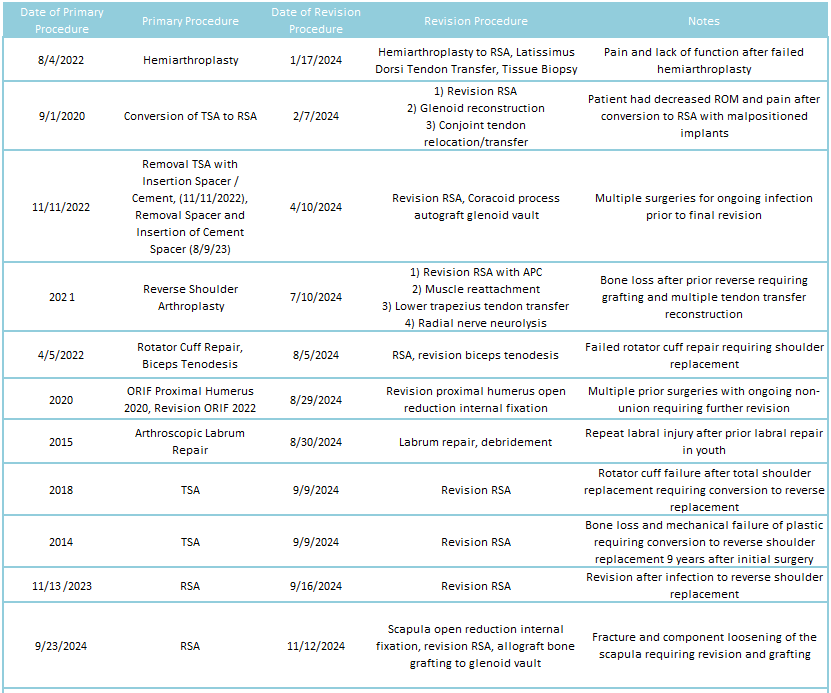
2024 Revisions of Dr. Lohre’s Cases

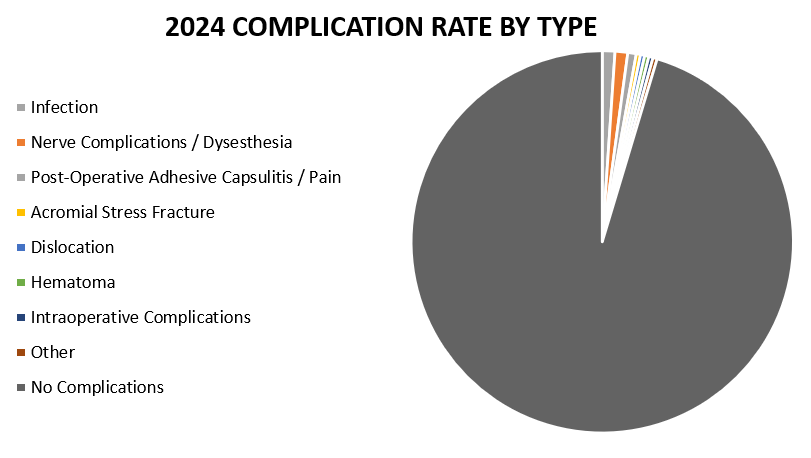
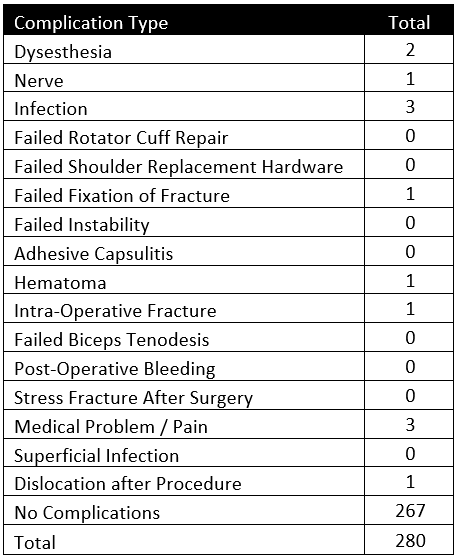
2024 Complications Overview
Of 280 patients operated on by Dr. Lohre in 2024, 13 patients (4.6%) experienced a complication during or after surgery. These complications were identified in 2024. Of the 13 complications, 6 required additional surgeries, while the overall reoperation rate was 2.1% (6 reoperations out of 280 patients operated). An explanation of each complication can be found below. Items in green were patients who had resolution of their complication and those indicated in red had an ongoing issue at the time of this reporting.
Infection
This patient underwent a Reverse Shoulder Arthroplasty procedure and displayed infection symptoms 10 days postoperatively. Patient underwent a subsequent Irrigation and Debridement procedure to wash out the infection. The patient is no longer displaying symptoms of infection
This patient underwent a hardware removal and elbow reconstruction surgery and developed symptoms of infection. Patient underwent a subsequent Irrigation and Debridement procedure and has recovered with no signs of infection.
This patient underwent a Pectoralis Major Transfer and developed an infection around their prior surgical site many months after their surgery. The patient underwent a subsequent Irrigation and Debridement procedure with removal of hardware. The patient has recovered with no signs of infection.
Nerve Complications / Dysesthesia
This patient underwent a revision Hemiarthroplasty to Reverse Shoulder procedure and has ongoing burning sensations around their surgical scar (no apparent nerve damage). Patient and was prescribed neuromodulating medications to address a superficial dysesthesia but continues to have sensitivity.
This patient underwent an Arthroscopic Nerve Release surgery and felt significant burning sensations around the shoulder due to intraoperative nerve compression. The patient was prescribed pregabalin and therapy to address their nerve pain. Despite not fully resolved, the patient’s dysesthesias have significantly improved.
This patient underwent a Rotator Cuff Repair procedure and deltoid paralysis due to damage of the axillary nerve. The cause of the nerve damage is not clear since all precautions were taken to not damage the nerve intraoperatively. The patient is still recovering, and further workup is in progress.
Post-Operative Adhesive Capsulitis / Pain
This patient underwent a revision Reverse Shoulder Arthroplasty to replace the prosthesis with titanium components due to a discovered allergy to cobalt and nickel. The patient continued to have significant pain even after switching components and underwent an additional revision procedure. Patient has significantly improved with no symptoms of pain.
This patient developed elbow tendonitis after a revision of a failed TSA to a reverse replacement. The patient has been limited to at-home exercises and has gotten progressively worse with a steroid injection to the elbow. Patient was given a wrist splint to help alleviate the pain.
Acromial Stress Fracture
This patient developed a stress fracture of the acromion after a Reverse Shoulder Replacement and is currently recovering with immobilization.
Dislocation
This patient underwent a revision Reverse Shoulder Arthroplasty procedure and sustained a dislocation of the prosthesis. The patient underwent a subsequent revision Reverse Shoulder Arthroplasty and the patient’s dislocation has now been corrected and all symptoms of instability resolved.
Hematoma
This patient received an Irrigation and Debridement procedure to wash out a postoperative hematoma. The patient has recovered without any further problems.
Intraoperative Complications
This patient was originally planned for a Reverse Shoulder Arthroplasty but instead received a temporary replacement (Hemi-Reverse Shoulder Replacement) due to sustaining a glenoid fracture secondary to very poor bone quality. The patient is awaiting a second stage conversion to a Reverse Shoulder Arthroplasty but is managing symptoms well in the interim.
Other
This patient underwent a complex Reverse Shoulder Arthroplasty procedure and had a fracture postoperatively due to significantly inadequate care from caregivers, lifting the patient by the operative arm. The patient received a subsequent Revision to Hemiarthroplasty procedure and has improved significantly. The patient is quite happy with their shoulder and can perform tasks pain free.
