2024 Outcomes Report (Dr. Warner)
One of the core values of our service is measurement and transparency. Thus, every year we review all surgical cases performed by physicians on our service and report these publicly for prospective and current patients to review as they wish. This is a short-term review as we perform longer-term analysis for publication and for cohort reporting for all patients separate from this report. By measuring outcomes, we can analyze our treatment in order to continually improve care.
Dr. Warner’s outcomes data is collected and compiled by the clinical research coordinator for the service, utilizing the electronic medical records system of Massachusetts General Hospital as well as surgical billing data. Our methodology consists of a review of all operations performed during the calendar year on a case-by-case basis, with special consideration made to procedure type, patient past surgical history (primary vs. revision status), and any complications arising during or after an operation. This data was collected, aggregated, and independently analyzed by the research coordinator with no direct input from the attending physician. The final review was performed by the surgeon in order to check accuracy of procedures and outcomes.
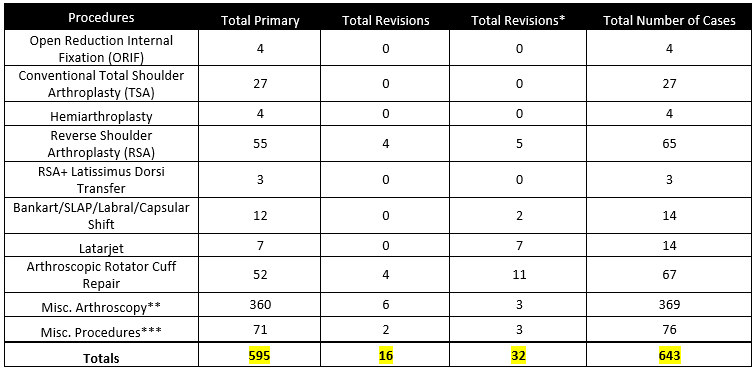
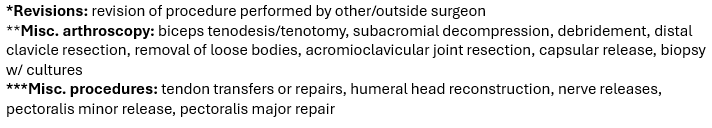
2024 Surgical Overview
The following section will provide an overview of all cases done by Dr. Warner in 2024. Importantly, procedures are not the same as total surgeries performed – one surgery may (and often does) include multiple procedures completed during the same operation. For example, a patient may undergo a shoulder arthroplasty and a biceps tendon tenodesis during the same surgery. These are recorded below as separate procedures, but as a single surgery.
- 643 procedures were performed on 242 patients by Dr. Warner during the 2024 calendar year across.
- Of these 643 procedures, 595 were primary procedures. A “primary” procedure refers to the first surgical intervention done for a patient’s condition. If Dr. Warner performs a rotator cuff repair on a patient who has not had a repair done on that shoulder yet, this would be considered a primary surgery. 16 of these procedures were revisions of his own past cases (these revisions were performed in 2024, but the primary procedure was done at a prior time time). 32 of these procedures were revisions of procedures performed by other/outside surgeons
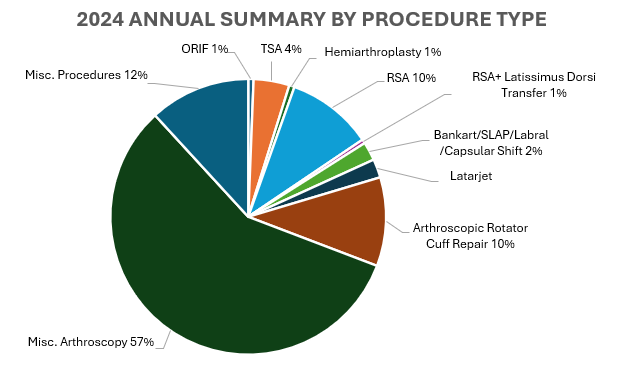

2024 Revision Descriptions
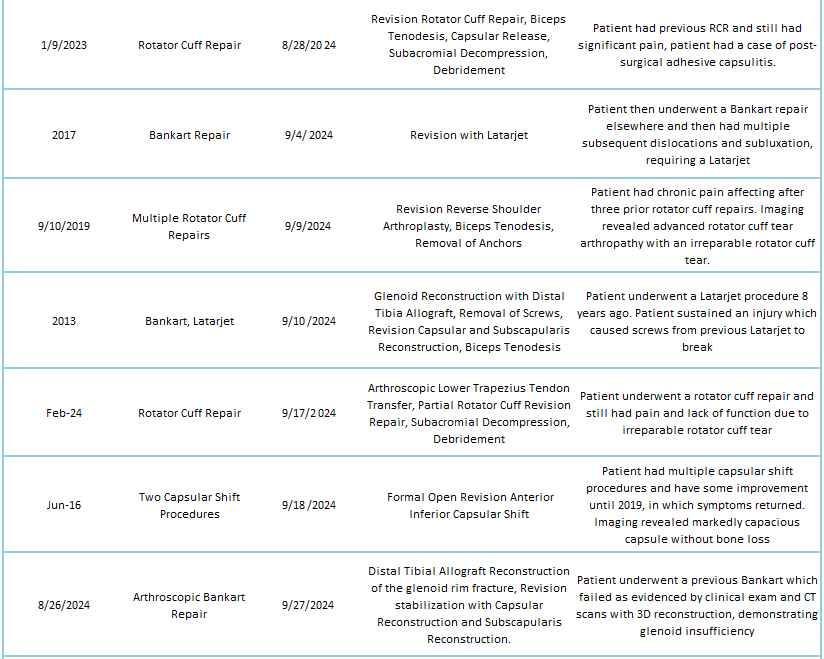
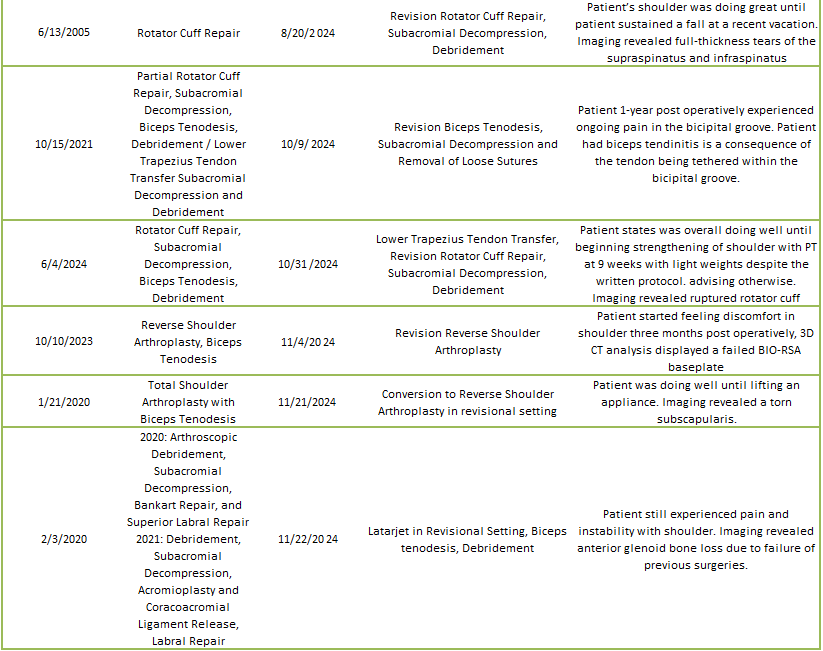
Of the 7% of Dr. Warner’s 2024 cases that were revisions, the average interval between primary and revision surgery was about 8.11 years. The shortest interval was 32 days, and the longest interval was 385 months or about 32 years. These revision procedures are summarized below:
2024 revisions for outside surgeons
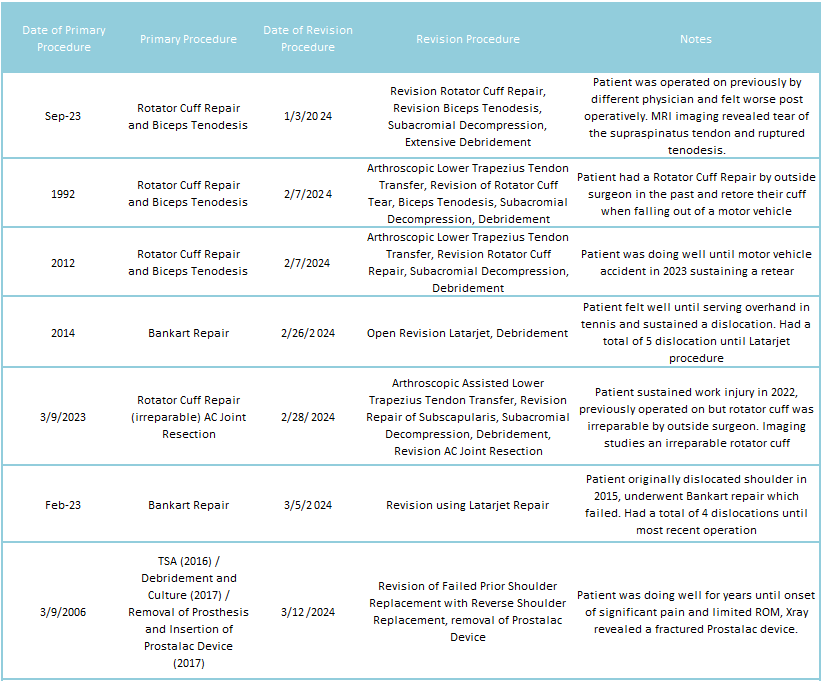

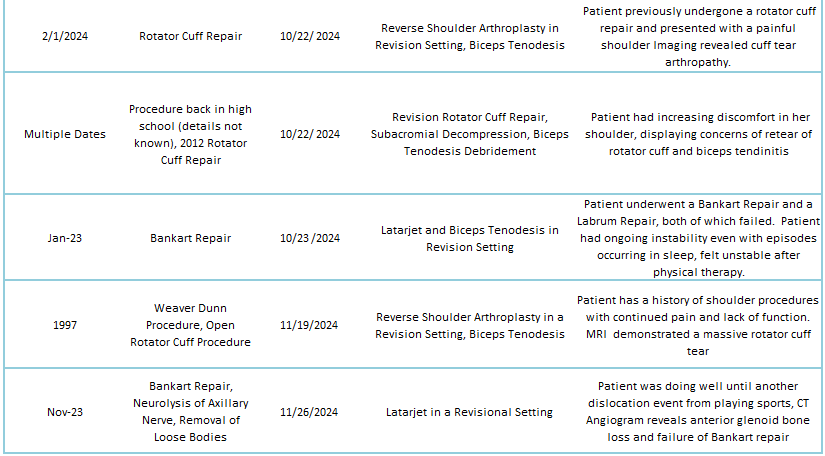
2024 revisions for Dr. Warner’s cases

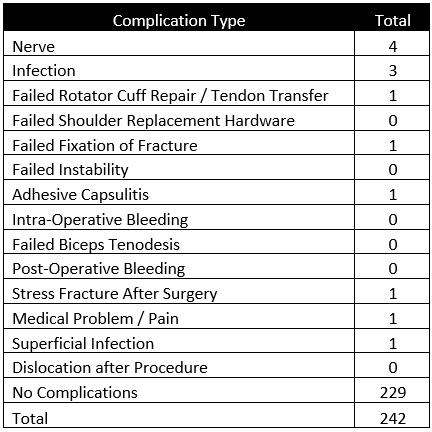
2024 Complications Overview
Of 242 patients operated on by Dr. Warner in 2024, 13 patients (5.4%) experienced a complication during or after surgery. These complications were identified in 2024. Of the 13 complications, 3 required additional surgeries, while the overall re-operation rate was 1.2% (3 reoperations out of 242). An explanation of each complication can be found below. Descriptions in green were patients who had resolution of their complication and those indicated in red have an ongoing issue at the time of this reporting.
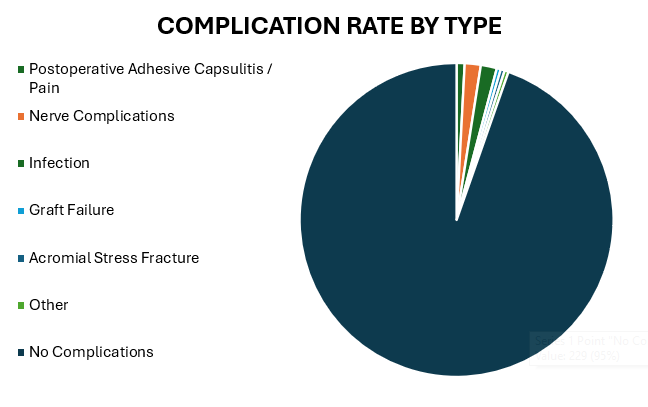
Postoperative Adhesive Capsulitis / Pain
This patient underwent Rotator Cuff Repair procedure which healed, however the patient developed postoperative adhesive capsulitis after the repair due to the setting of diabetes. The patient has significantly improved with physical therapy.
This patient continued to have anterior shoulder pain after receiving a Reverse Shoulder Procedure. Patient was referred to Dr. Elhassan for an additional procedure due to coracoid impingement. Fortunately, the patient’s pain has reduced significantly and can proceed with the procedure if symptoms return.
Nerve Complications
This patient had a previous Open Reduction and Internal Fixation procedure and experienced decreased sensation and strength of the deltoid. Patient improved with physical therapy and the neve issue completely resolved.
This patient underwent a Revision Total Shoulder replacement to Reverse Shoulder Arthroplasty procedure and developed hand numbness which has improved with therapy. The reverse replacement was successful.
This patient underwent an open Latarjet procedure and experienced stiffness and numbness postoperatively due to a stretch injury of the axillary nerve. The patient is has improved with therapy and was indicated for an additional capsule and nerve release procedures by Dr. Elhassan due to continue pain and stiffness.
This patient experienced temporary numbness after a Reverse Shoulder Arthroplasty procedure. Patient’s numbness has improved with therapy.
Infection
This patient after a Lower Trapezius Tendon Transfer procedure developed an infection and required a subsequent Irrigation and Debridement procedure to remediate the infection. Patient has no pain or symptoms of infection anymore.
This patient had a prior Prostalac implant placed for an infection and underwent a revision to Reverse replacement and now is happy and without pain.
This patient underwent a Sternoclavicular Joint Reconstruction procedure and had a superficial infection. Patient was treated with antibiotics and the symptoms resolved
This patient underwent a Reverse Shoulder Arthroplasty procedure with a Latissimus Dorsi tendon transfer and experienced infection-like symptoms two weeks postoperatively. Patient underwent a subsequent Irrigation and Debridement procedure and all symptoms of infection resolved.
Graft Failure
This patient underwent a Lower Trapezius Tendon Transfer procedure and the tendon transfer unfortunately failed. The patient was recommended a Reverse Shoulder Arthroplasty procedure if physical therapy fails, but the patient is doing well with therapy at this time
Acromial Stress Fracture
This patient underwent a Reverse Shoulder Arthroplasty procedure and developed significant pain in the shoulder postoperatively. Imaging revealed an acromial stress fracture and patient was advised to wear a sling for a month. Patient is doing much better now and returned to physical therapy
Other
This patient underwent a Total Shoulder Arthroplasty procedure for a severe malunion of the proximal humerus and still had significant pain and lack of function. Patient was asked to obtain an additional CT but hasn’t done so as of yet, lost to follow up
