Resection Arthroplasty of the Shoulder
Stephen Parada MD, Tamara Pylawka, Paul Yannopoulos, Jon JP Warner MD
September 29, 2013
What is resection arthroplasty?
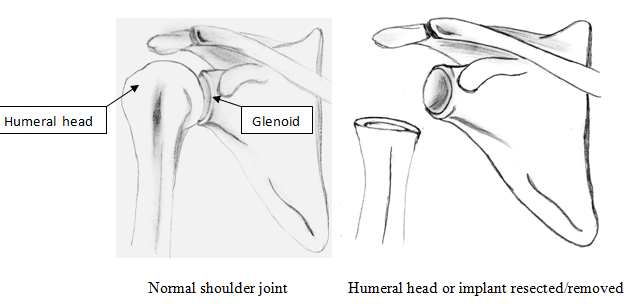
Resection arthroplasty is a procedure in which the humeral head or the prosthetic components (implants) are removed as a consequence of failed surgery, often in the setting of an infection. This is only performed when no other reconstructive options are possible.

When/ Why is a resection arthroplasty needed?
This procedure is a final salvage procedure, after multiple failed operations, when the patient has intolerable pain and poor function. It is often associated with infection after prior surgery and then failed reconstruction procedures. (see below)
- Persistent, chronic infection. To get rid of an infection that hasn’t responded to other treatments and surgeries, sometimes it is necessary to remove all components without placing anything else back in the shoulder. Postoperative infection for total shoulder arthroplasty (TSA) has been reported with a prevalence between 0-3.9%, and between 1-10% for reverse shoulder arthroplasty
- Failure of shoulder replacement. Failure can be due to loosening of the implants, instability of the implants or an actual mechanical failure of the implant. In all these cases, reconstruction is the first option, but if the bone quality or surrounding soft tissues won’t permit that, resection is the salvage procedure. (Fig. 1 and 2)
- Fracture with inability to repair bone because the bone quality is too poor.
- Severe arthritis or inflammatory arthritis like rheumatoid arthritis causing severe erosion of bone such that there is not enough bone to complete any reconstruction or implant
- Severe nerve injury(s) often in combination of one of the above situations.
Function of shoulder after resection arthroplasty: what patients should expect
Fig 1:
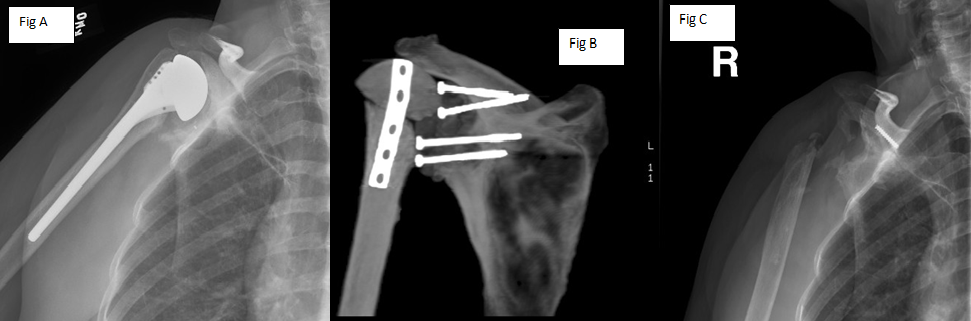
This patient had a total shoulder arthoplasty (Fig A) which became infected, so she had the components removed and a Prosthesis of Antibiotic Loaded Acrylic Cement placed (PROSTALAC – see module http://www.bosshin.com/prostalac). (Fig B). She also had IV antibiotics given for weeks but her infection could not be completely eliminated. Due to this, along with her severe pain, she had a resection arthroplasty performed (Fig C). See video of patient 1.
Fig 2:
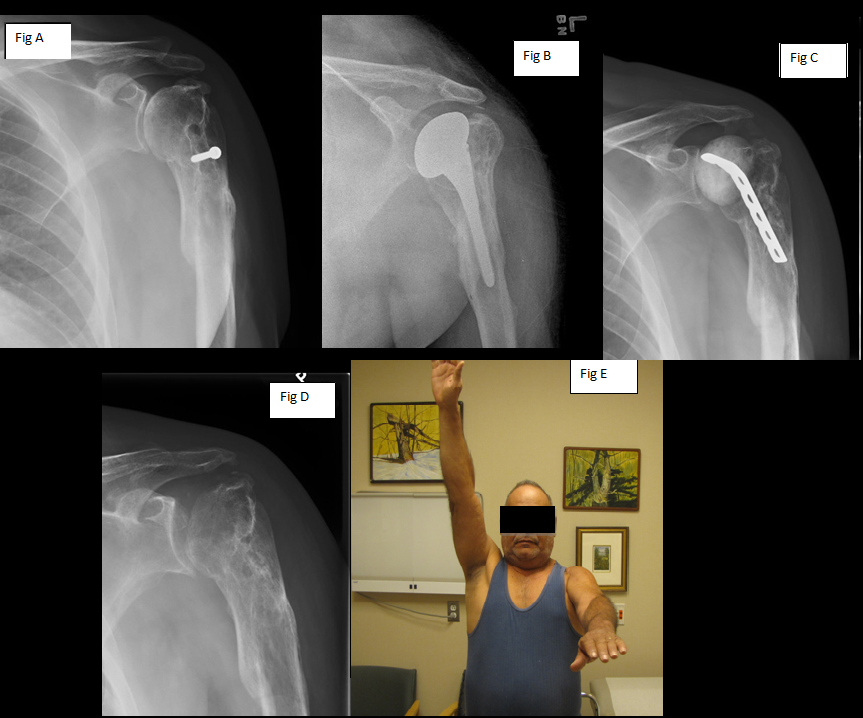
This patient had a fracture that had healed in an incorrect position and had a metal screw still in the humerus as well as arthritis in the shoulder (Fig A). He went on to have a hemiarthroplasty (replacement of just the humerus) for his pain and arthritis (Fig B). He developed an infection which was treated by removal of the component and placement of a PROSTALAC antibiotic cement spacer.(Fig C). Due to continued pain and inability to completely cure the infection, he had a resection arthroplasty performed (Fig D). This patient’s xrays demonstrate the variability in the amount of bone that is resected compared to the previous patient.
Six months after surgery, he is in 0/10 pain, reports that he feels his shoulder is 70% of normal and is happy with the results of the procedure. He is seen being able to lift his arm close to 90 degrees (Fig E). See video of patient 2.
How is resection arthroplasty completed?
Once it is determined that a resection arthroplasty is the best procedure to address pain, infection or fracture otherwise untreatable by other methods, the procedure is removal of the humeral head and / or glenoid component. After removal then no additional reconstructive efforts are made. The space between is left to have scar fill in. After humeral head resection, tissue forms between the remaining humeral head and glenoid. The formation of this scar tissue, is important for achieving a good functional result. The amount of the humeral head that is resected depends upon the patient’s operative history and how much was resected during past arthroplasty operations.
Results of Recent Studies on Resection Arthroplasty
- Braman JP, Sprague M, Bishop J, Lo IK, Lee EW, Flatow EL. The outcome of resection shoulder arthroplasty for recalcitrant shoulder infections. J Shoulder Elbow Surg. 2006 Sep-Oct;15(5):549-53
- http://www.ncbi.nlm.nih.gov/pubmed/16979048
- This study looked at outcomes of resection arthroplasty for shoulder infections that were recalcitrant to standard infection treatment protocols. In this series of seven patients, the average forward flexion was 28 degrees (range 0-80) and average external rotation was 8 degrees (range negative 20 to 40). In this study all patients reported that they could reach their mouth, arm pit on their opposite side and into their back pocket. All but one patient was satisfied with their results and the authors concluded that this procedure is a reasonable option as a salvage procedure when re-implantation of a prosthesis is not an option.
- Debeer P, Plasschaert H, Stuyck J. Resection arthroplasty of the infected shoulder: a salvage procedure for the elderly patient. Acta Orthop Belg. 2006 Apr;72(2):126-30.
- http://www.ncbi.nlm.nih.gov/pubmed/16768253
- This group reported on resection arthroplasty as a salvage procedure for infected TSA in seven elderly patients. The results of this study were excellent for removal of infection but functional outcomes measured by usual orthopaedic scores were poor.
- Rispoli DM, Sperling JW, Athwal GS, Schleck CD, Cofield RH. Pain relief and functional results after resection arthroplasty of the shoulder. J Bone Joint Surg Br. 2007 Sep;89(9):1184-7.
- http://www.ncbi.nlm.nih.gov/pubmed/17905955
- A study by the Mayo Clinic reported that reduction of pain is possible in one half to two thirds of patients. Relief from pain cannot be guaranteed, but the shoulder is usually comfortable at rest, although with profound functional limitations.
- Muh SJ, Streit JJ, Lenarz CJ, McCrum C, Wanner JP, Shishani Y, Moraga C, Nowinski RJ, Edwards TB, Warner JJ, Walch G, Gobezie R. Resection arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2013 Feb;22(2):247-52. doi: 10.1016/j.jse.2012.05.025
- http://www.ncbi.nlm.nih.gov/pubmed/22938790
- A multicenter study of five hospitals including Mass General Hospital, reported on 26 patients that had resection arthroplasty performed after failed shoulder arthroplasty (6 total shoulder arthroplasty cases, 7 hemiarthroplasty cases and 13 reverse shoulder arthroplasty cases.)
The authors reported that these patients had significant improvement with their pain going from a 6 (+/– 4) out of 10 to a 3 (+/– 2) out of 10. The average forward flexion was 45 degrees (+/- 30 degrees and external rotation to 9 degrees (+/- 13). The conclusions of this study indicated that resection arthroplasty is good at relieving pain, however patients can expect poor postoperative function. This study also showed that patients having a resection after a reverse TSA had the worst outcome. .
Conclusion
In conclusion, resection arthroplasty can be viewed as a last option after other procedures have failed and no other options are available for a patient to manage their pain. While this operation has been successful at decreasing pain levels, it may not completely eliminate pain. Following this operation, the patient never has a normal shoulder and has greatly decreased range of motion; however, many patients will perceive a dramatic reduction in their pain compared to their preoperative situation.
